
Quality of life instruments for survivors of brain injury from intimate partner violence: a scoping review
Highlight box
Key findings
• There are currently no quality of life (QOL) measures validated in survivors of intimate partner violence (IPV)-related brain injury.
• Medical Outcomes Study Short-Form 36-item (MOS SF-36) has been used multiple times in survivors of physical IPV.
What is known and what is new?
• IPV-related brain injury is a significant public health concern.
• QOL is a comprehensive framework to evaluate wellbeing in this population.
• Consider conducting validation and reliability studies on the MOS SF-36 with a sample of survivors of IPV-related brain injury.
What is the implication, and what should change now?
• Further research is needed to evaluate the validity and reliability of QOL measures in survivors of IPV-related brain injury.
• Screen for IPV in patients presenting to the emergency department with brain injuries and, likewise, screen for brain injury in survivors of IPV.
Introduction
Background
Intimate partner violence (IPV) is a significant public health concern that impacts people of all gender identities but disproportionately affects women (1,2). IPV refers to physically, psychologically, emotionally, sexually, or financially abusive behaviours that are directed towards a past or current intimate partner to exert power and control over them (3,4). Globally, it is estimated one in three women will experience IPV at some point in their life, with many survivors experiencing repeated instances of abuse within a relationship (5-7). In Canada, it is estimated to impact more than 44% of women and 33% of men who have been in an intimate relationship (8). Since the onset of the COVID-19 pandemic, the risk and incidence of IPV have increased due to heightened stress, disruption of protective services, stay-at-home orders, and restricted access to health care (9,10). IPV is therefore a widespread and urgent public health problem, which impacts the lives of individuals in complex ways.
Physical violence—which includes slapping, punching, shoving, pushing, kicking, and strangulation—is the most commonly experienced form of IPV (11). It often results in injuries to the head, neck, or face, which can increase the risk of sustaining a brain injury. A brain injury is defined as a disturbance in brain functioning that results from blunt force to the head, violent shaking, or asphyxiation (12). It is estimated between 30–74% of survivors of IPV sustain a brain injury from physical violence inflicted by an abuser, which is significantly higher than estimates of brain injuries incurred by athletes playing collision sports, which is approximately 10% (7,13-15) or the general population (16). While literature on brain injuries in athletes and veterans is available, research on brain injury in survivors of IPV is more limited or inconsistent (3), due in part to the barriers survivors encounter in disclosing such injuries. Brain injury is also a public health issue, which makes up a significant proportion of all emergency department visits (17).
Quality of life (QOL) is defined by the World Health Organization (WHO) as one’s opinion of their life situation, taking into account their culture, values, ambitions, expectations, standards, and worries (18). It is a multidimensional concept that considers the physical and mental health of an individual as well as their independence, relationships, beliefs, and their connection to various features of the environment (18). Thus, QOL is a holistic, subjective determination of the way in which various aspects of one’s own life are impacting functioning (18,19). QOL measures have been widely used in populations with brain injury from mechanisms other than IPV (e.g., sports, accidents, military). Many QOL measures, such as the Medical Outcomes Study Short-Form 36-item (MOS SF-36), have been validated in this population (19-21). In fact, there are QOL measures that have been developed specifically for this population, including the Traumatic Brain Injury-Quality of Life (TBI-QOL) measurement system (22).
Survivors of IPV-related brain injury are a unique population in that they have, by definition, survived both IPV and a brain injury. While each of these incidents comes with a range of biological, psychological, and social consequences (23,24), surviving both these traumas simultaneously has a unique, complex impact on the survivor, which is challenging to tease apart. It is important for researchers and practitioners to consider survivors of IPV-related brain injury have biopsychosocial circumstances that may differ from survivors of either IPV or brain injury in isolation. Therefore, evaluating the wellbeing of survivors of IPV-related brain injury requires a comprehensive framework. QOL measures provide this holistic assessment of wellbeing but a validated and reliable tool for this unique population is required.
Rationale and knowledge gap
Working through a trauma-informed lens, it is critical to identify strengths that contribute to an improved QOL among survivors of IPV-related brain injury, who quite often demonstrate profound resilience (25). Researchers therefore require instruments, including those measuring QOL, that have been validated in this population. Previous research has called for more comprehensive and validated evaluations of survivors of IPV-related brain injury (26,27).
Objective
The aim of this scoping review was to identify and evaluate the generalizability of instruments measuring QOL for use with survivors of IPV-related brain injury. We present this article in accordance with the PRISMA-ScR reporting checklist (available at https://jphe.amegroups.com/article/view/10.21037/jphe-23-120/rc).
Methods
Inclusion and exclusion criteria for studies in this scoping review
This review included studies that used or discussed an instrument measuring QOL and excluded those that did not. Qualitative, quantitative, and mixed-method peer-reviewed studies written in English were included. Given this is a relatively limited area of research, no exclusion criteria for geographical location was used, and no limiters on dates were applied. Finally, the age, gender, sex, sexual orientation, race, ethnicity, or socioeconomic status of participants were not considered in the inclusion or exclusion of articles. The initial search only included articles in which participants had experienced IPV-related brain injury. However, due to a lack of articles returned, eligibility criteria were expanded to include studies that measured QOL in participants who had survived some form of physical IPV, given this is associated with a high risk of sustaining a brain injury (28).
Search methods for identifying potential studies
This scoping review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) procedure (29). We conducted the search using the following databases accessed through the university library: Health and Psychosocial Instruments, PsychINFO, PubMed, CINAHL Complete, Social Work Abstracts, and Social Science Citation Index. The search was conducted between September 2019 and October 2019. Boolean search terms—such as “intimate partner violence”, “IPV”, “brain injury”, “TBI”, and “quality of life”—were used to gather articles matching at least one search term for each of the concepts, with the exception of the Health and Psychosocial Instruments journal in which articles matching at least one search term for either IPV or brain injury as well as QOL were gathered. This was done because no results were returned with one term for all three concepts and because of the relevance of the content in the Health and Psychosocial Instruments journal to our goal. See Table 1 for a complete list of the search terms by concept and Boolean operators used. Please note the term “battered women”, which is largely outdated, was used as a keyword to ensure older articles that used this terminology were included. At each step of this review, we conferred with an expert in brain injury research as well as a community member working with survivors of IPV. The final search terms were developed in collaboration with both experts, and were unanimously deemed representative of our aim.
Table 1
| Concept 1—QOL: “quality of life” AND Concept 2—IPV: “intimate partner violence” (OR “IPV” OR “domestic violence” OR “DV” OR “battered women” OR “spousal abuse” OR “domestic abuse” OR “spousal violence”) AND/OR† Concept 3—brain injury: “brain injury” (OR “TBI” OR “mTBI” OR concussion) |
†, the search input in all journals used the ‘AND’ operator between Concept 2 and Concept 3, with the exception of the search input for the Health and Psychosocial Instruments journal wherein the ‘OR’ operator was used. Example search term input: (“quality of life”) AND (“intimate partner violence” OR IPV OR “domestic violence” OR DV OR “battered women” OR “spousal abuse” OR “domestic abuse” OR “spousal violence”) AND/OR (“brain injury OR TBI OR mTBI OR concussion). TBI, traumatic brain injury; mTBI, mild traumatic brain injury.
Data collection and analysis
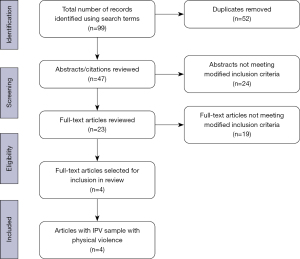
The initial search for measures of QOL yielded 99 articles. The results were exported to RefWorks, a reference management software program. Once all duplicates were removed, 47 articles remained, and each was reviewed. First, the titles and abstracts were reviewed. Articles with titles and abstracts that satisfied the inclusion/exclusion criteria (or had insufficient information in the title or abstract to determine eligibility) were included for full-text review. Next, the full text of each of the remaining articles was reviewed to determine whether they satisfied the inclusion/exclusion criteria. The full-text review yielded no articles that assessed QOL in survivors of IPV-related brain injury, indicating a significant lack of validated measures of QOL for survivors of IPV-related brain injury.
A second review of the 47 articles was therefore conducted with modified inclusion/exclusion criteria that included some form of physical IPV, given that estimates suggest between 30–74% of survivors of physical IPV sustain brain injuries (7,13,14). Given the objective of this study was to identify measures of QOL in survivors of IPV with brain injury, a new search with only the QOL and IPV search terms was not conducted. The articles from the initial review were deemed to be most representative of the objective of this study and were therefore screened for samples in which physical violence was assessed. In doing so, the scoping review would produce a starting point on which to develop and validate a measure of QOL appropriate for use with this population. Following the same process as described above, all 47 articles that remained after de-duplication were re-assessed for eligibility using the modified criteria. This second review yielded four articles that met the modified inclusion/exclusion criteria, and were therefore included in this review. See Figure 1 for a complete list of the number of articles included and excluded at each phase of the second review.
Results
The initial search yielded no studies examining QOL in survivors of IPV-related brain injury. As a result, we modified the inclusion/exclusion criteria to include some measure of QOL with survivors of physical IPV. Using the modified criteria, the second search yielded four articles. Of the articles included in this review, all four were quantitative studies, with one longitudinal experimental intervention (30) and three cross-sectional, descriptive studies (31-33). Each of these studies included a sample of physical IPV survivors. These four studies used consecutive, convenience, and purposive sampling, recruiting participants from domestic violence shelters, police family violence units, hospitals, and research centers. Table 2 depicts various characteristics of the studies included in this review.
Table 2
| Study authors | Study title | Methods | Participant recruitment | Sampling technique | Sample |
|---|---|---|---|---|---|
| McFarlane et al. 2000 | Intimate Partner Violence: A Gender Comparison | Cross-sectional, descriptive study | Persons intending to file assault charges against an intimate partner at a large urban police department (location not specified) | Consecutive | N=100 (90 women; 10 men) |
| Tavoli et al. 2016 |
Quality of life in women who were exposed to domestic violence during pregnancy | Cross-sectional, descriptive study | Pregnant women attending a teaching hospital in Lorestan, Iran | Consecutive | N=230 (all women) |
| Mouton et al. 1999 | The associations between health and domestic violence in older women: results of a pilot study | Cross-sectional, descriptive study | Women who presented for screening visits at the observational study arm of the WHI’s Newark, NJ site | Purposive, convenience | N=257 (all women) |
| Sullivan et al. 1994 | An advocacy intervention program for women with abusive partners: six-month follow-up | Longitudinal experimental intervention with random assignment | Women staying at least one night in a domestic violence shelter in a Midwestern city | Purposive, convenience | N=141 (all women) |
WHI, Women’s Health Initiative.
Measures of physical violence
The studies in this review were included because the participants were survivors of IPV and were screened for physical violence, and/or its severity, which, as previously mentioned, puts survivors at higher risk of sustaining a brain injury than athletes (7,13,14) and the general population (16). In these four studies, physical violence was assessed using the Severity of Violence Against Women Scale: Actual Violence Subscale (31), the Abuse Assessment Screen (33), the Domestic Violence Screening Questionnaire (32), and a modified version of Straus’ [1979] Violence subscale in the Conflict-Tactics Scales (30). Table 3 depicts the rationale for the inclusion of each study as well as the QOL instrument identified in each of them.
Table 3
| Study | QOL measure | IPV measure | Physical violence screening |
|---|---|---|---|
| McFarlane et al. 2000 | MOS SF-36 Health Survey | Severity of Violence Against Women Scale: Actual Violence Subscale | 100% of the sample had filed assault charges against an intimate partner |
| Tavoli et al. 2016 | MOS SF-36 Health Survey† | Abuse Assessment Screen | Provided outcomes for survivors of physical violence separately |
| Mouton et al. 1999 | MOS SF-36 Health Survey | Domestic Violence Screening Questionnaire | Provided outcomes for survivors of physical violence separately |
| Sullivan et al. 1994 | Andrews and Withey’s [1976] Quality of Life measure (Modified) | Modified version of Straus’ [1979] Violence subscale in the Conflict-Tactics Scale | High report of physical assault and injuries sustained |
†, Iranian version, which has been validated in this language [Montazeri et al., 2005 (34)]. QOL, quality of life; IPV, intimate partner violence; MOS SF-36, Medical Outcomes Study Short-Form 36-item.
Measures of QOL
Of the four articles included in this scoping review, three studies (31-33) used the MOS SF-36 Health Survey (35) and one study (30) employed a modified version of Andrews and Withey’s [1976] Quality of Life measure (see Table 3). The MOS SF-36 Health Survey is a QOL instrument comprised of 36 questions, distributed across 8 subscales: physical functioning, role limitations due to physical problems, social functioning, bodily pain, mental health, role limitations due to emotional problems, vitality, and general health perceptions (35,36). This instrument has been assessed for reliability, which has ranged from 0.34 to 0.94 in previous studies (31,37), as well as construct validity with factor analysis (31,38). Alternatively, a modified version of Andrews and Withey’s [1976] Quality of Life instrument was used in one study (30), in which 25 items relevant to the experiences of survivors of abuse were selected to estimate QOL, although the specific items selected were not specified. All studies administered the questionnaires in an interview format.
The MOS SF-36 Health Survey has been used with survivors of physical IPV (31-33). Among a sample of survivors of IPV, McFarlane et al. (31) found the MOS SF-36 Health Survey scale had high reliability (Cronbach’s alpha =0.82) (see Table 4). The MOS SF-36 scale also had reliability coefficients equal to or greater than 0.80 for each subscale, excluding the bodily pain scale and social functioning scale, which were found to have a reliability coefficient of 0.77 and 0.63, respectively (31). McFarlane et al. (31) did not examine validity for the MOS SF-36 in the sample of physical IPV survivors. However, t-tests were used to examine the differences in scores between men and women. Study scores were then compared to population norm data. Of note, female survivors of IPV reported below normal scores for 7 of 8 scales, and male survivors of IPV reported lower than normal scores for 3 of 8 scales on the MOS SF-36 Health Survey. Both male and female survivors showed near normal scores for physical functioning (31).
Table 4
| Study | QOL measure | Reliability | Validity |
|---|---|---|---|
| McFarlane et al. 2000 | MOS SF-36 Health Survey | Cronbach’s alpha =0.82 | Not evaluated |
| Tavoli et al. 2016 | MOS SF-36 Health Survey† | Not evaluated | Not evaluated but state the instrument has been previously validated in healthy samples |
| Mouton et al. 1999 | MOS SF-36 Health Survey | Not evaluated | Not evaluated but state the instrument has been previously validated in healthy samples |
†, Iranian version, which has been validated in this language [Montazeri et al., 2005 (34)]. MOS SF-36, Medical Outcomes Study Short-Form 36-item; IPV, intimate partner violence; QOL, quality of life.
Tavoli et al. (33) and Mouton et al. (32) also used the MOS SF-36 but did not report reliability estimates or discuss validity for the sample. Instead, Tavoli et al. (33) and Mouton et al. (32) provided evidence the version of the MOS SF-36 used had been validated among a healthy sample of individuals (34,39). Mouton et al. (32) also reported overall scale scores for the sample were standardized to general population using linear t-score transformation. It should also be noted Tavoli et al. (33) were using the Iranian version of the MOS SF-36, whereas Mouton et al. (32) and McFarlane et al. (31) were using the English version.
Finally, QOL was also assessed using a modified version of the Andrews and Withey’s [1976] Quality of Life measure, as part of a longitudinal intervention study of IPV survivors (30). Among this sample of IPV survivors, rates of physical violence were high (e.g., 76% reported being physical harmed). This 25-item measure showed high internal consistency (Cronbach’s alpha =0.90), with low to moderate item-total correlations (r=0.30–0.65).
Discussion
Key findings
This scoping review found no studies evaluating QOL in survivors of IPV-related brain injury. While the lack of studies measuring QOL in survivors of IPV-related brain injury limits the generalizability of any existing instrument to this population, it also highlights a significant gap in the literature and lack of validated measures. There are currently no instruments assessing QOL that have been validated for this unique population with complex situations. As such, there is limited ability to assess the myriad of outcomes survivors of IPV-related brain injury may experience. QOL is a multifaceted concept that is well suited for this population as it provides a comprehensive assessment of wellbeing. This concept moves away from the medical model, which is typically deficit-focused, and considers both areas of concern as well as strengths. From a research perspective, it allows investigators to identify areas of strengths and needs for this population, upon which interventions may build. It is therefore imperative the reliability, validity, and sensitivity of an existing instrument be assessed or, alternatively, a new and specific measure be developed.
As the initial review did not yield any studies evaluating QOL in survivors of IPV-related brain injury, a second review was conducted using modified inclusion/exclusion criteria, which included studies with a sample of survivors of physical IPV. After full text review using the modified criteria, four studies with samples of IPV survivors screened for physical violence were included in this review. While brain injury was not assessed in any of the studies, the exposure to physical abuse puts the participants in these studies at higher risk of having sustained such an injury (28). Therefore, the results must be evaluated with the understanding the samples are survivors physical IPV and not necessarily survivors of IPV-related brain injury.
Among the studies included in this review, two instruments measuring QOL were identified: the MOS SF-36 Health Survey and a modified version of Andrews and Withey’s [1976] Quality of Life measure. Both instruments were administered through an interview in all studies, which may be important for survey completion, at the risk of imposing interviewer bias. While the reliability and validity of both instruments in survivors of IPV with brain injury is inconclusive, the MOS SF-36 was used multiple times in survivors of physical IPV (31-33) and was found to have high reliability (31), whereas a modified version Andrews and Withey’s [1976] Quality of Life measure was only found to have been used in this population once and the items selected were not specified (30). The studies included in this review provide preliminary insight into the generalizability of the MOS SF-36 Health Survey to survivors of physical IPV injury, while also highlighting the need for further analysis with survivors of IPV-related brain injury. Of the studies included in this review that used the MOS SF-36 Health Survey, only one evaluated the reliability of the instrument and found high reliability (Cronbach’s alpha =0.82), which is at the upper end of the 0.43 to 0.94 reliability range found in previous studies (31). The other two studies did not report the reliability of the MOS SF-36 Health Survey (32,33). None of the studies using the MOS SF-36 Health Survey elaborated on the validity of the measure in their sample (31-33). Tavoli et al. (33) and Mouton et al. (32), however, indicate the instrument had been previously validated in healthy samples. Future studies may consider conducting validation and reliability studies on the MOS SF-36 with a sample of survivors of IPV-related brain injury. The addition of a brain injury may impact the degree to which items are relevant to survivors, and may require modification to get a true assessment of QOL with this population.
Strengths and limitations
This is the first study to investigate QOL measures in survivors of IPV-related brain injury. The results of this study highlight a significant gap in the literature and provide direction for future research to validate QOL measures in this unique population. Furthermore, this study followed the PRISMA procedure to perform a systematic investigation of existing literature. This study advocates for wellbeing among a population impacted by a pressing public health concern.
The results and recommendations for a measure of QOL should be considered with the following limitations in mind. The initial search for QOL measurement among survivors of IPV-related brain injury yielded no articles, resulting in the use of a secondary, more liberal, strategy to include additional articles. In particular, the inclusion criteria were expanded to include articles with participants who had survived physical IPV. We therefore reviewed studies that may have a sample comparable to survivors of IPV-related brain injury, but this sample was not screened for brain injury. Furthermore, without a specific measure of brain injury, we are unable to determine the severity of the brain injury. The severity, as well as the number and recency of brain injuries, may influence the ability of participants to answer questions on a survey or during an interview related to QOL. More importantly, QOL may change over time and be affected by brain injury severity. This further highlights the importance of using a validated and reliable measure of QOL among survivors of IPV-related brain injury.
Comparison with similar research
QOL measures have been validated and are widely used with those living with brain injury. The TBI-QOL measurement system is a tool developed to assess QOL specifically in those with traumatic brain injury, addressing several domains subjectively important to individuals with traumatic brain injury (22). However, the items of this tool may not reflect the key concerns of survivors of IPV-related brain injury. For instance, survivors of IPV-related brain injury may be facing other issues, such as actively fleeing violence while caring for children and living in unstable housing, which take precedence over those directly related to brain injury. While the TBI-QOL has been specifically developed for survivors of traumatic brain injury, it may not be an appropriate tool for evaluating QOL in survivors of IPV-related brain injury.
Sociodemographic characteristics of samples
While this review aimed to include studies with samples of diverse gender and sexual orientation, all samples were comprised of women only, with the exception of one study, which compared IPV between men and women, and included 10 men (31). All the studies also focused on heterosexual relationships. This may be partly due to the sampling techniques—whereby participants were recruited at healthcare appointments, domestic violence shelters, and police stations while filing charges—given differences in help-seeking behaviours across genders and sexual orientation (40,41). Furthermore, some studies in this review excluded participants with mental disorders (30,33), which may be problematic given the prevalence of mental health disorders and substance use in survivors of IPV and brain injury (7,14,42-44). McPherson and Martin (45) suggest that the SF-36 Health Survey is suitable for use with an alcohol-dependent population but cautioned no studies were found to analyze it with this population. Therefore, it is imperative studies also assess the validity and reliability of this instrument in samples wherein survivors of IPV-related brain injury with mental disorders and substance use are not excluded.
Implications and actions needed
Future research should consider the validity and reliability of QOL measures among survivors of IPV-related brain injury. Validated and reliable QOL measures for survivors of IPV-related brain injury would allow for comparison of QOL in survivors of IPV with a confirmed brain injury with other populations, such as survivors of IPV without brain injury or survivors of brain injury sustained from mechanisms other than IPV. This research would also permit the identification of any items in the measure addressing difficulties associated specifically with either IPV or brain injuries. For instance, items related to symptoms of brain injury, such as dizziness and difficulty concentrating, may be important to include.
Despite the limited and inconsistent results, the MOS SF-36 Health Survey is an instrument that should be considered for further testing regarding the reliability, validity, and sensitivity among survivors of IPV-related brain injury. Ultimately, this instrument should be tested among survivors of IPV-related brain injury to determine if any items or testing approaches require modification for use with this population.
Conclusions
To fully understand this growing public health concern, there must be a validated and reliable measure to assess a full range of outcomes following IPV-related brain injury. Yet, the initial review in this study revealed a measure of QOL has yet to be validated among survivors of IPV-related brain injury, suggesting a significant gap in the literature with direct impacts on practice and research. In spite of this lack of validation, this review identified the MOS SF-36 Health Survey has been used in survivors of physical IPV and may be adaptable for survivors of IPV-related brain injury (31-33). The MOS SF-36 Health Survey has also been used in samples with brain injury (19-21,46). EXPAND Future research must determine the validity and reliability of the MOS SF-36 for survivors of IPV-related brain injury, which may involve modifying items or using a data collection approach to address the unique needs of this population (see Table 5). In validating a measure of QOL designed for survivors of IPV-related brain injury, the development process should include the involvement of survivors and front-line workers. This process may also provide a template for measure validation with other growing, yet unique, populations.
Table 5
| Topic | Recommendations |
|---|---|
| Research | • Assess for brain injury in survivors of IPV with physical violence, especially in patients presenting to emergency departments with brain injuries |
| • Evaluate the validity and reliability of instruments assessing QOL among survivors of IPV-related brain injury | |
| • Compare QOL in survivors of IPV-related brain injury to survivors of IPV without brain injury | |
| Practice | • Consider that survivors of IPV may have sustained a brain injury and understand the implications this has on QOL |
| • Train front-line workers to assess for brain injury in survivors of IPV and provide referrals to appropriate services | |
| • Encourage emergency department staff to screen patients with brain injury for IPV | |
| • Provide psychosocial services that are accessible to survivors of IPV living with a brain injury | |
| Policy | • Enact agency-level policies that require and monitor that practitioners screen for brain injury or IPV |
| • Implement programs to improve QOL in survivors of IPV-related brain injury | |
| • Fund research on QOL in survivors of IPV-related brain injury |
IPV, intimate partner violence; QOL, quality of life.
The validation of a reliable instrument would assist in promoting a strengths-based research and practice agenda. In research, it is critical to explore factors that promote wellbeing and improve our understanding of healing processes, which in turn informs public health practice and policy recommendations. Similarly, in practice, the development of meaningful public health interventions requires consideration of both the strengths and needs of this population. Furthermore, measuring QOL would enable practitioners to not only track progress related to the reduction of negative outcomes associated with IPV and brain injury, but also to highlight growth among survivors. This is especially relevant now, with the increased incidence of IPV during the COVID-19 pandemic, and the public health consequences this will have in the years to come.
Acknowledgments
Funding: This work was supported by funding from Women and Gender Equality Canada (No. GV18385 to P.v.D.), the Max Bell Foundation (No. MB 18-A-15 to P.v.D.), and an anonymous donor.
Footnote
Reporting Checklist: The authors have completed the PRISMA-ScR reporting checklist. Available at https://jphe.amegroups.com/article/view/10.21037/jphe-23-120/rc
Peer Review File: Available at https://jphe.amegroups.com/article/view/10.21037/jphe-23-120/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jphe.amegroups.com/article/view/10.21037/jphe-23-120/coif). P.v.D. reports fundings from Women and Gender Equality Canada, Max Bell Foundation, and an anonymous donor. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Statistics Canada. Family violence: How big is the problem in Canada? 2018. Available online: https://www.canada.ca/en/public-health/services/health-promotion/stop-family-violence/problem-canada.html
- Smith SG, Zhang X, Basile KC, et al. The National Intimate Partner and Sexual Violence Survey: 2015 data brief – updated release. Atlanta, GA, USA: National Center for Injury Prevention and Control; 2018.
- St Ivany A, Schminkey D. Intimate Partner Violence and Traumatic Brain Injury: State of the Science and Next Steps. Fam Community Health 2016;39:129-37. [Crossref] [PubMed]
- World Health Organization. Understanding and addressing violence against women: intimate partner violence. 2012.
- World Health Organization. Violence against women. 2021;
- Kwako LE, Glass N, Campbell J, et al. Traumatic brain injury in intimate partner violence: a critical review of outcomes and mechanisms. Trauma Violence Abuse 2011;12:115-26. [Crossref] [PubMed]
- Valera EM, Berenbaum H. Brain injury in battered women. J Consult Clin Psychol 2003;71:797-804. [Crossref] [PubMed]
- Cotter A. Intimate partner violence in Canada, 2018: An overview. Available online: https://www150.statcan.gc.ca/n1/pub/85-002-x/2021001/article/00003-eng.htm
- Sharma A, Borah SB. Covid-19 and Domestic Violence: an Indirect Path to Social and Economic Crisis. J Fam Violence 2022;37:759-65. [Crossref] [PubMed]
- World Health Organization. COVID-19 and violence against women: what the health sector/system can do. 2020.
- Black MC, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey: 2010 Summary Report. Atlanta, GA, USA: National Center for Injury Prevention and Control Centers for Disease Control and Prevention; 2011.
- Brain Injury Association of America. About brain injury: Brain injury basics. Available online: https://www.biausa.org/brain-injury/about-brain-injury/what-is-a-brain-injury
- Smirl JD, Jones KE, Copeland P, et al. Characterizing symptoms of traumatic brain injury in survivors of intimate partner violence. Brain Inj 2019;33:1529-38. [Crossref] [PubMed]
- Cimino AN, Yi G, Patch M, et al. The Effect of Intimate Partner Violence and Probable Traumatic Brain Injury on Mental Health Outcomes for Black Women. J Aggress Maltreat Trauma 2019;28:714-31. [Crossref] [PubMed]
- Pierpoint LA, Collins C. Epidemiology of Sport-Related Concussion. Clin Sports Med 2021;40:1-18. [Crossref] [PubMed]
- Frost RB, Farrer TJ, Primosch M, et al. Prevalence of traumatic brain injury in the general adult population: a meta-analysis. Neuroepidemiology 2013;40:154-9. [Crossref] [PubMed]
- Taylor CA, Bell JM, Breiding MJ, et al. Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths - United States, 2007 and 2013. MMWR Surveill Summ 2017;66:1-16. [Crossref] [PubMed]
- The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med 1995;41:1403-9. [Crossref] [PubMed]
- Polinder S, Haagsma JA, van Klaveren D, et al. Health-related quality of life after TBI: a systematic review of study design, instruments, measurement properties, and outcome. Popul Health Metr 2015;13:4. [Crossref] [PubMed]
- Guilfoyle MR, Seeley HM, Corteen E, et al. Assessing quality of life after traumatic brain injury: examination of the short form 36 health survey. J Neurotrauma 2010;27:2173-81. [Crossref] [PubMed]
- Findler M, Cantor J, Haddad L, et al. The reliability and validity of the SF-36 health survey questionnaire for use with individuals with traumatic brain injury. Brain Inj 2001;15:715-23. [Crossref] [PubMed]
- Tulsky DS, Kisala PA. An Overview of the Traumatic Brain Injury-Quality of Life (TBI-QOL) Measurement System. J Head Trauma Rehabil 2019;34:281-8. [Crossref] [PubMed]
- Alsaker K, Moen BE, Kristoffersen K. Health-Related Quality of Life among Abused Women One Year after Leaving a Violent Partner. Soc Indic Res 2008;86:497-509. [Crossref]
- Fernández M, Verdugo MÁ, Gómez LE, et al. Core Indicators to Assess Quality of Life in Population with Brain Injury. Soc Indic Res 2018;137:813-28. [Crossref]
- Howell KH, Thurston IB, Schwartz LE, et al. Protective Factors associated with Resilience in Women Exposed to Intimate Partner Violence. Psychol Violence 2018;8:438-47. [Crossref] [PubMed]
- Dow-Fleisner S, Harris-Gendron S, van Donkelaar P, et al. Assessing measures of resilience and posttraumatic growth for use among survivors of intimate partner violence-related brain injury: A scoping review. Transl Issues Psychol Sci 2023;9:160-79. [Crossref]
- Hunnicutt G, Lundgren K, Murray C, et al. The Intersection of Intimate Partner Violence and Traumatic Brain Injury: A Call for Interdisciplinary Research. J Fam Violence 2017;32:471-80. [Crossref]
- Zieman G, Bridwell A, Cárdenas JF. Traumatic Brain Injury in Domestic Violence Victims: A Retrospective Study at the Barrow Neurological Institute. J Neurotrauma 2017;34:876-80. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. [Crossref] [PubMed]
- Sullivan CM, Campbell R, Angelique H, et al. An advocacy intervention program for women with abusive partners: six-month follow-up. Am J Community Psychol 1994;22:101-22. [Crossref] [PubMed]
- McFarlane J, Willson P, Malecha A, et al. Intimate Partner Violence: A Gender Comparison. J Interpers Violence 2000;15:158-69. [Crossref]
- Mouton CP, Rovi S, Furniss K, et al. The associations between health and domestic violence in older women: results of a pilot study. J Womens Health Gend Based Med 1999;8:1173-9. [Crossref] [PubMed]
- Tavoli Z, Tavoli A, Amirpour R, et al. Quality of life in women who were exposed to domestic violence during pregnancy. BMC Pregnancy Childbirth 2016;16:19. [Crossref] [PubMed]
- Montazeri A, Goshtasebi A, Vahdaninia M, et al. The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res 2005;14:875-82. [Crossref] [PubMed]
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473-83. [Crossref] [PubMed]
- Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976) 2000;25:3130-9. [Crossref] [PubMed]
- Ware JE, Snow KK, Kosinski M, et al. SF-36 health survey: manual and interpretation guide. Boston, MA, USA: The Health Institute, New England Medical Center; 1993.
- McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993;31:247-63. [Crossref] [PubMed]
- Ware JE, Kosinski MA, Keller SD, et al. SF-36 physical and mental health summary scales: a user's manual. Boston, MA, USA: The Health Institute, New England Medical Center; 1994.
- Donovan C, Hester M. Domestic Violence and Sexuality: What’s Love Got to Do with It? 1st edition. Bristol: Policy Press; 2014.
- Machado A, Santos A, Graham-Kevan N, et al. Exploring Help Seeking Experiences of Male Victims of Female Perpetrators of IPV. J Fam Violence 2017;32:513-23. [Crossref]
- Hink AB, Toschlog E, Waibel B, et al. Risks go beyond the violence: Association between intimate partner violence, mental illness, and substance abuse among females admitted to a rural Level I trauma center. J Trauma Acute Care Surg 2015;79:709-14; discussion 715-6. [Crossref] [PubMed]
- Kreutzer JS, Seel RT, Gourley E. The prevalence and symptom rates of depression after traumatic brain injury: a comprehensive examination. Brain Inj 2001;15:563-76. [Crossref] [PubMed]
- Ponsford J, Whelan-Goodinson R, Bahar-Fuchs A. Alcohol and drug use following traumatic brain injury: a prospective study. Brain Inj 2007;21:1385-92. [Crossref] [PubMed]
- McPherson A, Martin CR. A review of the measurement properties of the 36-item short-form health survey (SF-36) to determine its suitability for use in an alcohol-dependent population. J Psychiatr Ment Health Nurs 2013;20:114-23. [Crossref] [PubMed]
- von Steinbuechel N, Covic A, Polinder S, et al. Assessment of Health-Related Quality of Life after TBI: Comparison of a Disease-Specific (QOLIBRI) with a Generic (SF-36) Instrument. Behav Neurol 2016;2016:7928014. [Crossref] [PubMed]
Cite this article as: Harris-Gendron S, Dow-Fleisner S, van Donkelaar P, Mason K. Quality of life instruments for survivors of brain injury from intimate partner violence: a scoping review. J Public Health Emerg 2023;7:32.


