
Psychological impacts of the COVID-19 pandemic on nurses and coping strategies: a systematic review
Highlight box
Key findings
• This study was described the psychological impact that occurs on nurses and the types of coping strategies used by nurses in dealing with the COVID-19 pandemic.
• The high number of negative psychological problems that occur in nurses during a pandemic, increases the risk of mental illness in nurses.
What is known and what is new?
• The risk factors for the emergence of psychological problems experienced by nurses during the COVID-19 pandemic can be mostly associated with the demographic conditions.
• Nurses used positive attitudes towards stressful situations and psychological counseling as coping strategies for psychological problems experienced.
What is the implication, and what should change now?
• The COVID-19 pandemic impact on mental conditions of nurses ranging from stress, feeling fear, depression, sadness and anger.
• Appropriate and effective positive coping strategies can maintain the mental health and quality of life of nurses.
Introduction
Background
Coronavirus disease 2019 (COVID-19) where the first case was found in Wuhan, Hubei Province, China in 2019 became a world crisis problem because it spread very quickly. In March 2020, COVID-19 spread around the world so quickly that the World Health Organization (WHO) officially declared it a world pandemic (1). Until June 2023, it was approximately 767,750,853 confirmed cases, a total of 6,941,095 deaths have been reported almost worldwide (2). Even though large-scale social restrictions have been carried out and the implementation of strict health protocols, the rate of spread of the COVID-19 virus has not been significantly reduced (3). Until June 2023, it was reported that 2,087 health care workers (HCWs) in Indonesia died from COVID-19, of which there were 670 nurses (4).
Rationale and knowledge gap
The rapid spread, high infection rates and even death have an impact on the psychology of nurses as the frontline such as experiencing anxiety, stress and depression (5). Data shows that during the COVID-19 pandemic the number of nurses who experienced acute stress was 64%, depression was 53% and anxiety was 40% (6). In addition, nurses also experience fear and even desire to leave their jobs (7). Nurses sometimes choose to hide the fact that they work in a COVID-19 isolation ward (8). Nurses in Indonesia also experience psychological impacts during the pandemic as happened at the West Sumatera Pulmonary Hospital, namely stress, severe anxiety, to depression (9). Other symptoms that are often experienced by nurses are anxiety, excessive worry, fear of infection, difficulty concentrating, disappointment and doubt that result in psychological stress (10). If this is not managed properly, it is feared that they will experience acute stress disorder which puts them at risk for post-traumatic stress disorder or post-traumatic stress disorder (PTSD), decreased immunity and decreased work productivity (11).
The COVID-19 pandemic situation requires nurses’ psychological adaptations that depend on their assessment of the situation and behavior, whether to continue to face reality or avoid this outbreak. Responding to this situation, each individual is different in responding to it (12). Coping strategies will affect a person’s emotions or thoughts in order to produce a good quality of life and produce a positive action, but if the use of coping strategies is not appropriate, it can produce severe psychological stress (13). Nurses have their own coping strategies in dealing with pandemic situations such as in New York, 80% of nurses use coping strategies to manage stress by choosing physical activities/exercises (59%) and implementing virtual group spiritual practices (16%) (6). Thus, someone who uses coping strategies will experience lower stress (14). There are similar studies that have been carried out, but healthcare workers fighting against COVID-19 with study limitations in the western region do not focus on nurses in the wider world region (15). This study also expands the database and data period used by previous similar studies (16).
Objective
Based on this background, the researchers were interested in being to explore and describe the psychological impact that occurs on nurses and the types of coping strategies used by nurses in dealing with the COVID-19 pandemic reported in the literature. We present this article in accordance with the PRISMA reporting checklist (available at https://jphe.amegroups.com/article/view/10.21037/jphe-22-57/rc) (17).
Methods
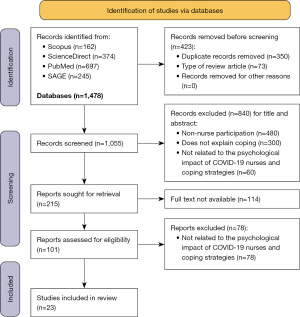
The type of research used is a systematic review through searching for articles in four databases, namely Scopus, PubMed, ScienceDirect and SAGE, the literature review focuses on the psychological impact of the COVID-19 pandemic on nurses and coping strategies. Literature review involves finding, reading, understanding and forming conclusions about the published research and theory and presenting it in an organized manner (18).
Eligibility criteria
The search used four databases from Scopus, PubMed, ScienceDirect and SAGE. The search is limited, namely from January 2020 to December 2022. Search literature using keywords that are adjusted to the Medical Subject Heading (MeSH) namely ((psychological) OR (mental AND health) OR (psychological AND stress) AND (impact) OR (effect) OR (disturbance) AND (COVID-19) OR (coronavirus AND disease 2019) OR (sars AND cov-2) OR (novel AND coronavirus AND disease) AND (nurse) OR (nurses) AND (coping AND strategies) OR (emotional AND adjustment) OR (coping AND behavior) OR (coping AND adaptation)). We included articles that were: (I) published in English, (II) published in a peer-reviewed journal, and (III) published in an original article form. We excluded studies that were not related to coping strategies and emotional states of nurses during the COVID-19 pandemic.
Study selection
Based on the results of a literature search on four databases using keywords that have been adapted to MeSH, the researchers identified 400 journals. Then three reviewers (Nihayati HE, Pratiwi IN and Santus R) independently screened all identified articles based on the January 2020 to December 2022 limit and using English the results are 1,478 articles, including Scopus (n=162), ScienceDirect (n=374), PubMed (n=697) and SAGE (n=245). The next step is to select the duplication of the four databases (n=423). The next stage is eligibility by excluding titles and abstracts whose research subjects are non-nurse participation (n=480), does not explain coping (n=300), not related to the psychological impact of COVID-19 nurses and coping strategies (n=60) so that 215 article titles and relevant abstracts were obtained. The next stage is to search for the availability of full text articles and exclude full text articles that do not discuss the psychological impact of COVID-19 nurses and coping strategies (n=78) so that articles that are included full text can be analyzed (n=23) (Figure 1) (19). Any disagreement between the two reviewers during the screening process was discussed until a consensus was reached.
Quality assessment
Articles that met the inclusion criteria were independently assessed by three reviewers (Nihayati HE, Pratiwi IN and Santus R) for methodological validity prior to inclusion in the review using The Joanna Briggs Institute’s (JBI) Critical Assessment Checklist for several types of correlational (20) and qualitative studies (21). The JBI-based checklist lists several questions to assess the quality of the study. The assessment criteria are given a score of “yes”, “no”, “unclear” or “not applicable”, and each “yes” score is assigned one point and the other scores are zero. Each score is then calculated and summed. If the research score is at least 50% it meets the critical appraisal at the cut-off point. The risk of bias in this literature review uses an assessment of the research methods of each study, namely in the aspects of theory, design, samples, variables, instruments and data analysis used.
Results
Assessment criteria study results
Table 1 shows the results of a literature review search that obtained 23 articles that passed the screening according to the criteria that have been determined based on JBI Critical Appraisal Tools (41).
Table 1
| No | Author [year] | Criteria | Results | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||
| 1 | Ali et al. [2020] (22) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 2 | Al Muharraq [2021] (23) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 3 | Babore et al. [2020] (12) | x | √ | √ | √ | √ | √ | √ | √ | 7/8 (88%) | ||
| 4 | Chen et al. [2020] (24) | √ | √ | √ | √ | x | x | √ | √ | 6/8 (75%) | ||
| 5 | Dal’Bosco et al. [2020] (25) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 6 | Eftekhar Ardebili et al. [2021] (26) | √ | √ | √ | √ | √ | x | √ | √ | √ | √ | 9/10 (90%) |
| 7 | Habibi Soola et al. [2022] (27) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 8 | Huang et al. [2020] (28) | √ | √ | √ | √ | √ | x | √ | √ | 7/8 (88%) | ||
| 9 | Jubin et al. [2022] (29) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 10 | Kackin et al. [2021] (30) | √ | √ | √ | √ | √ | x | √ | √ | √ | √ | 9/10 (90%) |
| 11 | Kang et al. [2020] (31) | x | √ | √ | √ | √ | √ | √ | √ | 7/8 (88%) | ||
| 12 | Kowalczuk et al. [2022] (32) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 13 | Lorente et al. [2021] (33) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 14 | Maideen et al. [2022] (34) | √ | √ | √ | √ | √ | x | √ | √ | √ | √ | 9/10 (90%) |
| 15 | Maiorano et al. [2020] (35) | x | √ | √ | √ | √ | √ | √ | √ | 7/8 (88%) | ||
| 16 | Man et al. [2020] (36) | x | √ | √ | √ | √ | √ | √ | √ | 7/8 (88%) | ||
| 17 | Peiró et al. [2020] (37) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 18 | Shechter et al. [2020] (6) | x | √ | √ | √ | √ | √ | √ | √ | 7/8 (88%) | ||
| 19 | Salopek-Žiha et al. [2020] (38) | x | √ | √ | √ | √ | √ | √ | √ | 7/8 (88%) | ||
| 20 | Shahrour et al. [2020] (39) | √ | √ | √ | √ | √ | √ | √ | √ | 8/8 (100%) | ||
| 21 | Sun et al. [2020] (8) | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | 10/10 (100%) |
| 22 | Zhang et al. [2020] (7) | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | 9/10 (90%) |
| 23 | Zhang et al. [2021] (40) | √ | √ | √ | √ | √ | x | x | √ | √ | √ | 8/10 (80%) |
The results of critical appraisal in Table 1 use The JBI Critical Appraisal Tools, where 17 articles use the JBI critical appraisal checklist for analytical cross-sectional studies with a total score of 8 and 6 articles use the JBI critical appraisal checklist for qualitative studies with a total score of 10 points. The value of criteria 1 to 10 is the number of critical appraisal questions in The JBI Critical Appraisal Tools according to the research design of each article. The symbol “yes” (√) is eligible and the symbol “no” (×) is not eligible. Nine articles with the checklist for analytical cross-sectional studies received a “yes” rating of 8 out of a total score of 8 or 100% (8/8) with good quality and seven articles that received an answer/rating of “no” were all on the first question 7/8 (88%) good quality. There are six qualitative studies with a total criteria of questions 1–10, where only 1 article received two “no” ratings with a score of 8/10 (80%) but still categorized as good quality. The results of the study review of the 23 articles achieved a higher score of more than 50% so that it met the critical appraisal which will then be analyzed for data.
Characteristics of the selected studies
Table 2 shows the results obtained by 23 articles with 2020–2022 limitations and using English which consists of 17 articles with cross-sectional studies and 6 articles with qualitative studies. Six articles are from China including Wuhan, where COVID-19 started, two articles are from Italy, USA, Spain and Iran. The rest are spread by one article each from Turkey, Romania, Croatia, Jordan, Brazil, Saudi Arabia, France, Poland, Belarus, and Brunei Darussalam.
Table 2
| No. | First author [year] | Design | Country | Participants | Objective | Instruments |
|---|---|---|---|---|---|---|
| 1 | Ali et al. [2020] (22) | Cross-sectional study | Alabama, USA | 109 nurses | To investigate the major stressors and coping strategies reported by nurses working directly with potentially infectious patients during the COVID-19 pandemic | The questionnaire instrument consisted of four components: a demographic and work-related data component, a stressor-scale component, nurses feelings component and coping strategies component |
| 2 | Al Muharraq [2021] (23) | Cross-sectional study | Jazan, Saudi Arabia | 215 frontline nurses | To explore the psychological impact of coronavirus disease 2019 on frontline nurses and their coping strategies | The questionnaire divided into 5 different sections: (I) the demographic characteristics; (II) the feelings of participants during the outbreak; (III) potential factors that could cause stress; (IV) factors that could help in reducing stress; (V) coping strategies |
| 3 | Babore et al. [2020] (12) | Cross-sectional study | Italy | 595 health workers (261 nurses) | To analyse the impact of COVID-19 outbreak on healthcare professionals and the coping strategies used to deal with stress | Online questionnaire: socio-demographical and professional data, PSS and coping strategies (COPE-NVI-25) |
| 4 | Chen et al. [2020] (24) | Cross-sectional study | Wuhan, China | 92 nurses | To evaluate the mental health status, stressors and self-adjustment of nurses in isolation wards at different periods | Questionnaires: sociodemography, self-reporting questionnaire-20, mental condition assessment, self-reported stressors and incidents questionnaire, self-adjustment questionnaire |
| 5 | Dal’Bosco et al. [2020] (25) | Cross-sectional study | Paraná, Brazil | 88 nurses | To identify prevalence and factors associated with anxiety and depression in nursing professionals who work to cope with COVID-19 at a university hospital | Hospital Anxiety and Depression Scale by Zigmond and Snaith |
| 6 | Eftekhar Ardebili et al. [2021] (26) | Qualitative study | Iran | 36 nurses | To undertake an in-depth exploration of the experiences of healthcare staff working during the COVID-19 crisis | In-depth interviews |
| 7 | Habibi Soola et al. [2022] (27) | Cross-sectional study | Iran | 494 ED/EMS nurses | To explores the spiritual coping (positive or negative) among ED nurses and EMS staff during the COVID-19 pandemic | Demographic information form and spiritual coping questionnaire |
| 8 | Huang et al. [2020] (28) | Cross-sectional study | China | 374 nurses and 430 nursing students | To investigate nurses’ emotional responses and coping styles, and conduct a comparative study with nursing college students | COPE Brief Questionnaire prepared by Carver [1997] and positive and negative emotion scale (PANAS) |
| 9 | Jubin et al. [2022] (29) | Cross-sectional study | France | 9,898 nurses | To identify the protective factors they mobilized to face the crisis and how these factors contributed to sustaining their QoL | QoL (WHOQOL-BREF), perceived stress (PSS-14), resilience (CD-RISC), social support (MSPSS), and coping style (Biref-COPE) questionnaires |
| 10 | Kackin et al. [2021] (30) | Qualitative study | Istanbul, Turkey | 10 nurses | To determine the experiences and psychosocial problems of nurses caring for patients diagnosed with COVID-19 |
In-depth interview |
| 11 | Kang et al. [2020] (31) | Cross-sectional study | Wuhan, China | 994 doctors and nurses (811 nurses) | To explore the mental health status of medical and nursing staff and the efficacy, or lack thereof, of critically connecting psychological needs to receiving psychological care | Questionnaire: sociodemography, PHQ-9, GAD-7, ISI, and IES-R |
| 12 | Kowalczuk et al. [2022] (32) | Cross-sectional study | Poland and Belarus | 284 nurses | To investigate and compare how nurses cope with stress during the COVID-19 pandemic | Mini-Cope inventory |
| 13 | Lorente et al. [2021] (33) | Cross-sectional study | Spain | 421 nurses | Effect of sources of stress during the peak of COVID-19 pandemic on nurses’ psychological distress, focusing on the mediating role of coping strategies | Nursing Stress Scale, the brief COPE, the resilience scale, and DASS-21 |
| 14 | Maideen et al. [2022] (34) | Qualitative study | Brunei Darussalam | 75 nurses | To explored nurses’ mental health and coping strategies working with suspected and confirmed COVID-19 patients | In-depth interview |
| 15 | Maiorano et al. [2020] (35) | Cross-sectional study | Italy | 240 health workers (66 nurses) | To investigated the direct and mediated effects of coping strategies and hardiness on secondary trauma | online questionnaire: DRS-15, CSES-SF, ESQ and STSS-I |
| 16 | Man et al. [2020] (36) | Cross-sectional study | Cluj-Napoca, Romania | 115 medical personnel including 40 nurses | To evaluate disease perceptions, levels of stress, emotional distress, and coping strategies among medical staff (COVID-19 versus non-COVID-19 departments) in a tertiary pulmonology teaching hospital in the first month after the outbreak of COVID-19 | Questionnaires: IPQ, PSS-10, PDE, and CERQ |
| 17 | Peiró et al. [2020] (37) | Cross-sectional study | Spain | 403 nurses | Drawing lessons for nursing education, the present study analyzed, during the weeks of peak infection in Spain, the stress experience and coping strategies | COPE: PFC and seeking support (SSC), CFA |
| 18 | Shechter et al. [2020] (6) | Cross-sectional study | New York, NY, USA | 657 health workers with 313 nurses | This study reports the sources and degrees of COVID-19-related distress that healthcare workers are experiencing, their current coping behaviors, and the wellness resources they believe may help | Questionnaire: PC-PTSD, PHQ-2, GAD-2, Life Orientation Test-Revised, PSQI and Insomnia Severity Index |
| 19 | Salopek-Žiha et al. [2020] (38) | Cross-sectional study | Croatia | 124 (97 nurses and 27 doctors) | To explore ways to deal with the coronavirus stressor and psychological outcomes among physicians and nurses | Questionnaire: SF-36 demographic characteristics, DASS-21 and Ways of Coping Questionnaire |
| 20 | Shahrour et al. [2020] (39) | Cross-sectional study | Jordan | 448 nurses | To establish the prevalence of acute stress disorder and predictors of psychological distress among | Web-based questionnaire/survey: SASRQ, Trauma Coping Self-efficacy and BSI-18 represented by Cronbach’s |
| 21 | Sun et al. [2020] (8) | Qualitative study | Henan Province, China | 20 nurses | To explore the psychology of nurses caring for COVID-19 patients | In-depth interview |
| 22 | Zhang et al. [2020] (7) | Qualitative study | Wuhan, China | 23 nurses | To identify the psychological change process of the registered nurses who worked in the epicenter of the COVID-19 outbreak | In-depth interview |
| 23 | Zhang et al. [2021] (40) | Qualitative study | China | 10 nurses | To explore the psychological changes of nurses during home isolation, the factors that related with these changes, and coping strategies in home isolation during the epidemic of COVID-19 | In-depth interview |
COVID-19, coronavirus disease 2019; ED, emergency department; EMS, emergency medical services; COPE, Coping Orientation to Problems Experienced; PSS, Perceived Stress Scale; COPE-NVI-25, Coping Orientation to Problem Experienced-New Italian Version-25; PANAS, Positive and Negative Affect Schedule; QoL, quality of life; WHOQOL-BREF, World Health Organization Quality-of-Life Scale; CD-RISC, Connor-Davidson Resilience Scale; MSPSS, Multidimensional Scale of Perceived Social Support; Biref-COPE, Coping Orientation to Problems Experienced Inventory; PHQ-9, 9-item Patient Health Questionnaire; GAD-7, 7-item Generalized Anxiety Disorder; ISI, Insomnia Severity Index; IES-R, Impact of Event Scale-Revised; DASS-21, Depression Anxiety Stress Scales-21; DRS-15, Dispositional Resilience Scale-15, Italian version; CSES-SF, Coping Self-Efficacy Scale-Short Form; ESQ, Emergency Stress Questionnaire; STSS-I, Secondary Traumatic Stress Scale-Italian Version; IPQ, Illness Perception Questionnaire; PDE, Profile of Emotional Distress; CERQ, Cognitive-Emotional Coping Questionnaire; PFC, problem-focused coping; SSC, support-seeking coping; CFA, confirmatory factor analysis; PC-PTSD, primary care post-traumatic stress disorder; PSQI, Pittsburgh Sleep Quality Index; SF-36, 36-Item Short Form Health Survey; DASS-21, 21-item Depression Anxiety Stress Scales; SASRQ, Stanford Acute Stress Reaction Questionnaire; BSI-18, Brief Symptom Inventory-18.
The psychological impact during the COVID-19 pandemic
From a total of 23 articles obtained, all agreed that frontline nurses dealing with COVID-19 pose a threat to mental health (Table 3). The psychological impacts experienced by nurses during the COVID-19 pandemic were 16 studies reporting stress (6,7,12,22,24,27,29-37,39) both emergency stress (35) to acute stress disorder (39) which are at risk of predisposing to PTSD (26), then 9 studies reported experiencing anxiety (22,23,25,26,28,30,31,34,38), six studies reported feeling fear (7,26,28,31,34,37), five studies reported depression (6,25,26,31,38), three studies reported sadness (28,30,31), two studies reported anger (28,31) and two studies reported burnout (26,34).
Table 3
| No. | First author [year] | Psychological impact by nurses during the COVID-19 pandemic | Coping strategies |
|---|---|---|---|
| 1 | Ali et al. [2020] (22) | Younger and less experienced nurses experienced greater levels of stress compared to senior or older nurses | Nurses use coping strategies by washing hands and wearing face masks and avoiding public transportation and crowded spaces |
| 2 | Al Muharraq [2021] (23) | Nurses reported being nervous and afraid at work and worried about transmitting the disease to their families | Nurses make efforts to follow strict protective measures and always keep abreast of the latest knowledge about COVID-19 |
| 3 | Babore et al. [2020] (12) | Risk factors that lead to nurse stress problems are low social support, lack of avoidance strategies and working with COVID-19 patients | A positive attitude towards stressful situations is the main protective factor for nurses working in the COVID-19 pandemic situation |
| 4 | Chen et al. [2020] (24) | Nurses feel under pressure and stress which appeared at 7–10 days and decreased after 60 days after they worked in the COVID-19 isolation room | Most nurses adjust to stress and use professional psychological counseling hotlines |
| 5 | Dal’Bosco et al. [2020] (25) | Nurses feel anxiety and depression which are also associated with their demographic profile such as; age, marital status, length of service, income and level of education | Nurses need psychological support, telephone counseling services that can be done anytime and confidentially, and relaxation exercises through yoga, reiki and others |
| 6 | Eftekhar Ardebili et al. [2021] (26) | Nurses experience moments of early exposure (fear, anxiety, loss of control), peak crises (anxiety, helplessness, hopelessness and depression) and long-term effects (depression, PTSD and burnout) | Nurses adapt to the situation experienced by complying with protocols, using personal protective equipment and taking precautions to prevent transmission |
| 7 | Habibi Soola et al. [2022] (27) | Nurses experienced stressful experiences during the pandemic which were exacerbated by older age, overtime work, and marital status | Nurses apply positive religious behavior as the main spiritual coping strategy |
| 8 | Huang et al. [2020] (28) | Frontline nurses experience stronger anxiety, fear, sadness, and anger | Nurses need more psychological support, adopt better training in coping strategies, arrange adequate medical protective equipment, and develop various interventions to block the spread of the virus |
| 9 | Jubin et al. [2022] (29) | Stressful conditions of denial, self-blame, substance use, and behavioral disengagement are associated with poor quality of life | Acceptance and framing coping strategies positively affect quality of life |
| 10 | Kackin et al. [2021] (30) | Nurses looked sad because of the high death rate due to COVID-19, so nurses admitted that they were anxious and stressed | Coping strategies used in the short term include: exercising, watching television, cooking, painting, listening to music and trying to divert attention by not thinking about the COVID-19 incident and using psychological consulting services |
| 11 | Kang et al. [2020] (31) | Nurses experienced mental health disorders; mild mental health disorders, moderate and experienced severe disorders | Efforts were made to overcome mental problems; accessing psychological materials through books on mental health, accessing psychological resources available through the media, and attending counseling or psychotherapy |
| 12 | Kowalczuk et al. [2022] (32) | Polish and Belorussian nurses experiencing stress in the face of the COVID-19 pandemic | The most frequently used coping strategies were active strategies (active coping, planning) and the least-used were avoidance strategies (behavioral disengagement, substance use) in both countries |
| 13 | Lorente et al. [2021] (33) | Nurses experience stress in a pandemic situation due to fear of infection, many patient deaths, and excessive workload | In achieving adaptive mental health behavior, nurses need two coping mechanisms (problem-focused coping or emotion-focused coping) and resilience resources |
| 14 | Maideen et al. [2022] (34) | Nurses experience self-emotional changes ranging from anxiety, fear, workload stress, sleep disturbances, loneliness, exhaustion and burnout | Self-care management is the most widely adopted strategy by nurses, which involves the use of spiritual coping, physical exercise, and yoga |
| 15 | Maiorano et al. [2020] (35) | Direct contact with COVID-19 patients, female gender, unexpected events, and lack of PPE are risk factors for emergency stress for nurses | The nurse’s coping strategies in emergency situations refer to personal resources, for example, a sense of self-efficacy in dealing with critical situations or events, and resilience |
| 16 | Man et al. [2020] (36) | Health workers experience high levels of stress and psychological pressure during the first month after the COVID-19 pandemic outbreak | Problem-focused coping strategies can predict emotional responses to some extent. The most common coping mechanisms are positive reassessment and a refocus on planning |
| 17 | Peiró et al. [2020] (37) | Nurses with long and extensive work experience protect against the stress of overwork situations, inadequate preparation, and fear of infection | Nurses use coping behaviors that focus on problems and find sources of support through seeking knowledge and skills related to pandemics and public health crises |
| 18 | Shechter et al. [2020] (6) | Psychological conditions found in nurses who treat patients with COVID-19, namely acute stress, depression, and symptoms of anxiety (33%) | Coping strategies carried out by nurses include doing physical activities/sports, and the rest doing independent counseling to online therapists |
| 19 | Salopek-Žiha et al. [2020] (38) | Mental problems experienced by health workers during the COVID-19 pandemic were moderate to very severe depression, moderate to very severe anxiety, moderate to very severe stress and the rest felt worried | Nurses use coping strategies and positive assessment with seeking social support and stress management techniques |
| 20 | Shahrour et al. [2020] (39) | Majority nurses experienced acute stress disorder due to the COVID-19 pandemic which was at risk of predisposing to PTSD | Coping mechanisms through increasing self-efficacy in preventing ASD and PTSD, through giving consecutive days off, allocating complex patient care rotations, availability of PPE, organizing psychological support services and making it accessible to staff |
| 21 | Sun et al. [2020] (8) | During the COVID-19 pandemic, positive and negative emotions from frontline nurses intertwine and coexist. In the early stages, negative emotions dominate then positive emotions appear gradually | Self-coping strategies and psychological growth in a positive direction play an important role in nurses such as confidence, calm, relaxation, and happiness, which simultaneously or gradually appear with negative emotions |
| 22 | Zhang et al. [2020] (7) | Nurses experience mental ambivalence such as fear of infection, emotional exhaustion which gets worse when nurses cannot seek support or talk directly to colleagues because close distances can cause cross-infection | Improved coping through energy renewal occurs 3–4 weeks after serving in the special COVID-19 room where nurses find meaning and are committed to professionalism so as to grow new energy |
| 23 | Zhang et al. [2021] (40) | Nurses experience many negative emotional reactions such as nervousness, fear, irritability, anxiety, panic, and worry in the early stages of isolation and positive emotions gradually increase during independent isolation at home | In this study, six categories of coping strategies that can be identified are reasoned cognition; autosuggestion; develop healthy protective behaviors; shifting attention; social support; and the power of a role model |
COVID-19, coronavirus disease 2019; PTSD, post-traumatic stress disorder; PPE, personal protective equipment; ASD, acute stress disorder.
The risk factors for the emergence of psychological problems experienced by nurses during the COVID-19 pandemic include the majority of which can be associated with the demographic conditions of nurses, namely the young age of nurses (22,25,39) and female gender (12,25,35). Then other causes of psychological problems that are felt are only in the early weeks of carrying out duties in the COVID-19 nation (24,28,36), direct contact with COVID-19 patients (25,35), low social support (12), lack of personal protective equipment (PPE) (35), low work experience (37), unmarried status, workload and shift arrangements and physical fatigue (25).
The types of coping strategies
In overcoming the psychological problems experienced by nurses during the COVID-19 pandemic, nurses used coping strategies (Table 3). The majority of studies reported that nurses used positive attitudes towards stressful situations (7,8,12,28,29,32,33,36,38,40) and psychological counseling (6,24,25,28,30,31,39) as coping strategies for psychological problems experienced. In addition, other coping strategies used by nurses are strengthening social support (24,28,31,38), complying with protocols, using PPE and taking precautions to prevent transmission, avoiding public transportation and crowded spaces (22,23,26,28), participating in training (28,37), exercising (6,30,34), watching television, cooking, painting, listening to music (30), always keep abreast of the latest knowledge about COVID-19 (23), reading books on mental health (31) and positive religious behavior (27,34). Resilience and coping strategies play a protective role (35,40) and require safeguarding and provision of personal security measures (25,26).
Discussion
Key findings
During the early COVID-19 outbreak, nurses had various negative emotional experiences. The psychological impact experienced by nurses during the COVID-19 pandemic were varied, but can increase the risk of PTSD. This review also identified, resilience and coping strategies originating from internal and external sources play a protective role and require safeguards and the provision of personal security measures.
Strengths and limitations
In general, the information obtained from the findings of this study can help nurses to effectively cope with the mental challenges caused by the COVID-19 pandemic through adequate coping strategies. The high number of negative psychological problems that occur in nurses during a pandemic, increases the risk of mental illness in nurses. It is important to provide psychological support through mental health screening and psychological condition counseling to deal with pandemic outbreaks in the future.
This review has included mostly cross-sectional studies (17 studies included), which may not establish a causal relationship between psychological problems and coping strategies used. More longitudinal studies are needed to show a significant relationship between psychological conditions and coping strategies that can be used. Another problem is that young female nurses are represented in most of the studies. Due to selection bias and overrepresentation of certain groups, most studies may not be representative of the original population. Importantly, studies on inclusion have only been conducted in a few countries. As a result, generalizations regarding mental health in the global nursing population cannot be made.
Apart from that, an article search for this review was also carried out mainly from the four medical databases Scopus, ScienceDirect, PubMed and SAGE. This database was chosen because it tends to be free in access and has flexibility. Relevant articles obtained from this search are not exhaustive, and searches on other databases may be performed in the future to gather more evidence on the subject.
Comparison with similar researches
During the COVID-19 pandemic, the nurse’s job situation became unusual where the demands of the job were high, with great responsibility and a strong commitment to work, so that it had an impact on psychological problems that affect mental health. This study aims to explore and describe the psychological impact that occurs on nurses and the types of coping strategies used by nurses in dealing with the COVID-19 pandemic through a literature review. There are similar studies that have been carried out, but healthcare workers fighting against COVID-19 with study limitations in the western region do not focus on nurses in the wider world region (15). This study focuses on nurses, in accordance with previous research that nurses play an important role in the health system which is 60% of the total health workforce and their contribution is very beneficial to public health (31). In dealing with the COVID-19 pandemic situation, in several studies relevant to this study where the symptoms that are often experienced by nurses are anxiety, excessive worry, fear of infection, difficulty concentrating, disappointment and doubt that results in psychological stress (10,16).
In this study focusing on the COVID-19 pandemic situation requires nurses’ psychological adaptations that depend on their assessment of the situation and behavior, whether to continue to face reality or avoid this outbreak. Responding to this situation, each individual is different in responding to it, which is relevant to several other studies (12,42,43). The results of this study are in line with other research that coping strategies will affect a person’s emotions or thoughts in order to produce a good quality of life and produce a positive action, but if the use of coping strategies is not appropriate, it can produce severe psychological stress (13).
Explanations of findings
All of the articles reviewed agree that nurses on the front lines dealing with COVID-19 pose a threat to mental health, nurses experience stress (6,7,12,22,24,27,29-37,39) both emergency stress (35) to acute stress disorder (39) which are at risk of predisposing to PTSD. The prevalence of among health workers dealing with disasters, including nurses, ranged from 14.6% (44). Nurses caring for COVID-19 patients have an increased risk of experiencing secondary trauma symptoms (10,45). Follow-up of in nurses and preventing it from developing into PTSD requires referral to appropriate psychological services (39). It is necessary to implement urgent interventions aimed at increasing the activation of protective factors that can reduce and prevent the development of serious psychological consequences (35,42).
Other psychological impacts experienced by nurses who handle COVID-19 in the articles reviewed are feeling anxiety (22,23,25,26,28,30,31,34,38), fear (7,26,28,31,34,37), depression (6,25,26,31,38), sadness (28,30,31) and anger (28,31). In the early stages, negative emotions dominate then positive emotions appear gradually (7,8,40). Several studies have shown that individuals experience four stages of mental development when responding to stress, namely shock, followed by defense, resolution, and growth (40). Thirty-six-point-nine percent of nurses experienced mental health disorders below the threshold immediately after the COVID-19 epidemic occurred, which were divided into three categories, namely experiencing mild mental health disorders (34.4%), moderate (22.4%) and experiencing severe disorders (6.2%) (31).
Based on the results of the literature review, the risk factors for the emergence of psychological problems experienced by nurses during the COVID-19 pandemic can be mostly associated with the demographic conditions of nurses, namely the young age of nurses (22,25,39) and female gender (12,25,35). Young people are more likely to use ineffective coping strategies during an outbreak (46). One possibility is that brain aging affects emotional responses. Older adults were found to be less likely to exhibit negative emotional experiences (39). Many articles related to trauma due to psychological stress show that women have higher psychological distress than men (13,47). In addition, a greater number of women are represented in the nursing profession (48-50).
Then other causes of psychological problems that are felt are only in the early weeks of carrying out duties in the COVID-19 nation (24,28,36), direct contact with COVID-19 patients (25,35), low social support (12), lack of PPE (35), low work experience (37), unmarried status, workload and shift arrangements and physical fatigue (25). Mental health problems that arise in nurses who work in the covid isolation ward are stress (26.09%) which appears on the 7–10 days after they work in the room. Then the number of nurses experiencing stress decreased (9.30%) in the COVID-19 isolation ward after 60 days (24). The lack of PPE and the uncertainty experienced in the early phase produced a predictive effect in terms of increasing stress levels (35,43,51). Years of nursing experience are protective against stress from situations of overwork, inadequate preparation, and fear of infection (37).
In overcoming the psychological problems experienced by nurses during the COVID-19 pandemic, nurses use coping strategies. The majority of studies reported that nurses used positive attitudes towards stressful situations (7,8,12,28,29,32,33,36,38,40) and psychological counseling (6,24,25,28,30,31,39) as coping strategies for psychological problems experienced. Always be positive at work as a strategy with a great impact in reducing stress (12,52). Functional coping strategies allow individuals to reinterpret negative situations in a positive way, which is closely related to self-efficacy, greater psychological well-being, and better quality of life (12). Frontline nurses dealing with COVID-19 require special attention, so hospitals should offer timely counselling, identifying high-risk individuals with common screening tools (24,53,54).
Implications and actions needed
Coping strategies based on the literature obtained reveal that nurses make efforts to strengthen social support (24,28,31,38), washing hands, wearing face masks, avoiding public transportation and crowded spaces (22,28), participating in training (28,37), exercising (6,30,34), watching television, cooking, painting, listening to music (30) and reading books on mental health (31). Resilience and coping strategies play a protective role (35) and require safeguarding and provision of personal security measures (25). In addition, the existence of family support becomes an important part of the social support system and can effectively reduce negative emotions and encourage positive responses (55,56).
Regarding the mental problems experienced by nurses during the COVID-19 pandemic, there is a need for social and organizational support for adaptation to the situation that occurs. Previous experience with pandemics and similar training is suggested as a useful coping strategy for health workers during a pandemic, in addition to provision of PPE, testing kits, orientation of worker training, work shift arrangements, provision of online counseling, provision of food and accommodation and prompt payment of benefits by management health services to nurses, provision of rooms for online consultation with psychologists/psychiatrists and easy access to social facilities and religious activities are important protective measures.
Managers in health care organizations need to recognize that primary prevention is the key to the success of any intervention to contain and control any epidemic. Thus, regular training with such objectives needs to be planned, oriented and ongoing based on proven infection control measures. These measures need to be supported by the timely provision of protective equipment, medicines, testing facilities, vaccines, isolation facilities, clinical and mental health support, and the welfare of health workers.
Conclusions
The COVID-19 pandemic which quickly spreads and infects humans can cause a heavy psychological impact on nurses. This review can inform current and future research priorities in the psychological impact of nurses in dealing with the COVID-19 pandemic. The COVID-19 pandemic situation has had a negative psychological impact on nurses. Nurses experience mental conditions ranging from stress, feeling fear, depression, sadness and anger. Appropriate and effective positive coping strategies can maintain the mental health and quality of life of nurses. More and more extensive studies are still needed to understand the coping strategies that nurses can use for the level of mental health problems experienced during the COVID-19 pandemic. Nurses in clinical settings need to be given the role and reinforcement regarding effective coping strategies to deal with stress and burnout conditions during the COVID-19 pandemic.
Acknowledgments
The authors would like to acknowledge the authors of sources used in this study.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Li Ping Wong) for the series “Psychological and Physical Impacts of COVID-19 Pandemic” published in Journal of Public Health and Emergency. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://jphe.amegroups.com/article/view/10.21037/jphe-22-57/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jphe.amegroups.com/article/view/10.21037/jphe-22-57/coif). The series “Psychological and Physical Impacts of COVID-19 Pandemic” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jeong SA, Kim J. Factors influencing nurses' intention to care for patients with COVID-19: Focusing on positive psychological capital and nursing professionalism. PLoS One 2022;17:e0262786. [Crossref] [PubMed]
- WHO Coronavirus (COVID-19) Dashboard. World Health Organization (WHO); 2023. Available online: https://covid19.who.int/
- Tayal D, Mehta AK. The Struggle to Balance Work and Family Life During the COVID-19 Pandemic: Insights Based on the Situations of Working Women in Delhi. J Fam Issues 2023;44:1423-65. [Crossref] [PubMed]
- Statistics on Mortality of Indonesian Health Workers [Internet]. Indonesia Covid Report. Ministry of Health Indonesia; 2023. Available online: https://nakes.laporcovid19.org/statistik
- Nie A, Su X, Zhang S, et al. Psychological impact of COVID-19 outbreak on frontline nurses: A cross-sectional survey study. J Clin Nurs 2020;29:4217-26. [Crossref] [PubMed]
- Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry 2020;66:1-8. [Crossref] [PubMed]
- Zhang Y, Wei L, Li H, et al. The Psychological Change Process of Frontline Nurses Caring for Patients with COVID-19 during Its Outbreak. Issues Ment Health Nurs 2020;41:525-30. [Crossref] [PubMed]
- Sun N, Wei L, Shi S, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control 2020;48:592-8. [Crossref] [PubMed]
- Tanjung DA, Huriani E, Rahman D. Optimism and Psychological Distress in Nurses During the Covid-19 Pandemic. Jurnal Smart Keperawatan 2021;8:14-25. [Crossref]
- Lai J, Ma S, Wang Y, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open 2020;3:e203976. [Crossref] [PubMed]
- Clancy G, Gaisser DD, Wlasowicz GK. COVID-19 and mental health: Self-care for nursing staff. Nursing 2020;50:60-3. [Crossref] [PubMed]
- Babore A, Lombardi L, Viceconti ML, et al. Psychological effects of the COVID-2019 pandemic: Perceived stress and coping strategies among healthcare professionals. Psychiatry Res 2020;293:113366. [Crossref] [PubMed]
- Mashudi S, Yusuf A. Family Coping Strategies to Improve the Health of Family Members Living with Schizophrenia. Jurnal Ners 2021;16:67-73. [Crossref]
- Yin H, Huang S, Lv L. A Multilevel Analysis of Job Characteristics, Emotion Regulation, and Teacher Well-Being: A Job Demands-Resources Model. Front Psychol 2018;9:2395. [Crossref] [PubMed]
- Danet Danet A. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med Clin 2021;156:449-58. (Engl Ed). [Crossref]
- Ding X, Jian Z, Xu Y, et al. Psychological stress and coping strategies among frontline healthcare workers supporting patients with coronavirus disease 2019: a retrospective study and literature review. Ther Adv Respir Dis 2022;16:17534666221130215. [Crossref] [PubMed]
- Brink H, van der Walt C, van Rensburg G. Fundamentals of research methodology for health care professionals. 3rd edition. Cape Town: Juta Academic; 2012.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol (Engl Ed) 2021;74:790-9. [Crossref] [PubMed]
- Moola S, Munn Z, Tufanaru C, et al. Checklist for analytical cross sectional studies. Joanna Briggs Inst Rev Man 2017:1-7. Available online: http://joannabriggs.org/research/critical-appraisal-tools
- Joanna Briggs Institute. Checklist for Qualitative Research. Joanna Briggs Inst 2017;6. Available online: http://www.joannabriggs.org/assets/docs/critical-appraisal-tools/JBI_Critical_Appraisal-Checklist_for_Qualitative_Research.pdf
- Ali H, Cole A, Ahmed A, et al. Major Stressors and Coping Strategies of Frontline Nursing Staff During the Outbreak of Coronavirus Disease 2020 (COVID-19) in Alabama. J Multidiscip Healthc 2020;13:2057-68. [Crossref] [PubMed]
- Al Muharraq EH. The Psychological Impact of Coronavirus Disease 2019 on Nurses in Saudi Arabia and Their Coping Strategies. SAGE Open Nurs 2021;7:23779608211011322. [Crossref] [PubMed]
- Chen H, Sun L, Du Z, et al. A cross-sectional study of mental health status and self-psychological adjustment in nurses who supported Wuhan for fighting against the COVID-19. J Clin Nurs 2020;29:4161-70. [Crossref] [PubMed]
- Dal’Bosco EB, Messias Floriano LS, Vienscoski Skupien S, et al. Mental health of nursing in coping with COVID-19 at a regional university hospital. Rev Bras Enferm 2020;73:e20200434. [Crossref] [PubMed]
- Eftekhar Ardebili M, Naserbakht M, Bernstein C, et al. Healthcare providers experience of working during the COVID-19 pandemic: A qualitative study. Am J Infect Control 2021;49:547-54. [Crossref] [PubMed]
- Habibi Soola A, Mozaffari N, Mirzaei A. Spiritual Coping of Emergency Department Nurses and Emergency Medical Services Staff During the COVID-19 Pandemic in Iran: An Exploratory Study. J Relig Health 2022;61:1657-70. [Crossref] [PubMed]
- Huang L, Lei W, Xu F, et al. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: A comparative study. PLoS One 2020;15:e0237303. [Crossref] [PubMed]
- Jubin J, Delmas P, Gilles I, et al. Protective Factors and Coping Styles Associated with Quality of Life during the COVID-19 Pandemic: A Comparison of Hospital or Care Institution and Private Practice Nurses. Int J Environ Res Public Health 2022;19:7112. [Crossref] [PubMed]
- Kackin O, Ciydem E, Aci OS, et al. Experiences and psychosocial problems of nurses caring for patients diagnosed with COVID-19 in Turkey: A qualitative study. Int J Soc Psychiatry 2021;67:158-67. [Crossref] [PubMed]
- Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun 2020;87:11-7. [Crossref] [PubMed]
- Kowalczuk K, Shpakou A, Hermanowicz JM, et al. Strategies for Coping With Stress Used by Nurses in Poland and Belarus During the COVID-19 Pandemic. Front Psychiatry 2022;13:867148. [Crossref] [PubMed]
- Lorente L, Vera M, Peiró T. Nurses´ stressors and psychological distress during the COVID-19 pandemic: The mediating role of coping and resilience. J Adv Nurs 2021;77:1335-44. [Crossref] [PubMed]
- Maideen AA, Idris DR, Lupat A, et al. Nurses' mental health and coping strategies throughout COVID-19 outbreak: A nationwide qualitative study. Int J Ment Health Nurs 2022;31:1213-27. [Crossref] [PubMed]
- Maiorano T, Vagni M, Giostra V, et al. COVID-19: Risk factors and protective role of resilience and coping strategies for emergency stress and secondary trauma in medical staff and emergency workers—an online-based inquiry. Sustainability 2020;12:9004. [Crossref]
- Man MA, Toma C, Motoc NS, et al. Disease Perception and Coping with Emotional Distress During COVID-19 Pandemic: A Survey Among Medical Staff. Int J Environ Res Public Health 2020;17:4899. [Crossref] [PubMed]
- Peiró T, Lorente L, Vera M. The COVID-19 Crisis: Skills That Are Paramount to Build into Nursing Programs for Future Global Health Crisis. Int J Environ Res Public Health 2020;17:6532. [Crossref] [PubMed]
- Salopek-Žiha D, Hlavati M, Gvozdanović Z, et al. Differences in Distress and Coping with the COVID-19 Stressor in Nurses and Physicians. Psychiatr Danub 2020;32:287-93. [Crossref] [PubMed]
- Shahrour G, Dardas LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nurs Manag 2020;28:1686-95. [Crossref] [PubMed]
- Zhang MM, Niu N, Zhi XX, et al. Nurses' psychological changes and coping strategies during home isolation for the 2019 novel coronavirus in China: A qualitative study. J Adv Nurs 2021;77:308-17. [Crossref] [PubMed]
- The Joanna Briggs Institute. JBI’s critical appraisal tools assist in assessing the trustworthiness, relevance and results of published papers. [Internet]. The Joanna Briggs Institute. 2020. Available from: https://jbi.global/critical-appraisal-tools
- Pratiwi IN, Setiawan HW, Pawanis Z, et al. The Psychological Experience of Frontline Nurses Amid the COVID-19 Pandemic. Malaysian Journal of Medicine and Health Sciences 2022;18:107-14.
- Setiawan HW, Pratiwi IN, Nimah L, et al. Challenges for Healthcare Workers Caring for COVID-19 Patients in Indonesia: A Qualitative Study. Inquiry 2021;58:469580211060291. [Crossref] [PubMed]
- Biggs QM, Fullerton CS, Reeves JJ, et al. Acute stress disorder, depression, and tobacco use in disaster workers following 9/11. Am J Orthopsychiatry 2010;80:586-92. [Crossref] [PubMed]
- Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e17-8. [Crossref] [PubMed]
- Sim K, Huak Chan Y, Chong PN, et al. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res 2010;68:195-202. [Crossref] [PubMed]
- Hansen MC, Ghafoori B. Correlates of Psychological Distress among Urban TraumaExposed Adults: Influence of age and coping preferences. Psychol Trauma 2017;9:85-92. [Crossref] [PubMed]
- Limiñana-Gras RM, Sánchez-López MP, Román AISS, et al. Health and gender in female-dominated occupations: The case of male nurses. J Mens Stud 2013;21:135-48. [Crossref]
- Priyantini D, Nursalam N, Sukartini T. Analysis of Factors Affecting the Mental Health Crisis of Coronavirus Disease Infection in Java Island. Jurnal Ners 2021;16:60-6. [Crossref]
- Pratiwi IN, Pawanis Z, Hidayati L, Widyawati IY, Ni’Mah L, Sukartini T, et al. The role of a healthy-eating educational module during Ramadan in a community health centre. J Diabetes Nurs 2018;22:JDN013.
- Nyashanu M, Pfende F, Ekpenyong M. Exploring the challenges faced by frontline workers in health and social care amid the COVID-19 pandemic: experiences of frontline workers in the English Midlands region, UK. J Interprof Care 2020;34:655-61. [Crossref] [PubMed]
- Khalid I, Khalid TJ, Qabajah MR, et al. Healthcare Workers Emotions, Perceived Stressors and Coping Strategies During a MERS-CoV Outbreak. Clin Med Res 2016;14:7-14. [Crossref] [PubMed]
- Benjamin LS, Abishek BJS, Dewi YS, et al. Challenges of Online Education among University Students, Saudi Arabia. Jurnal Ners 2021;16:188-92. [Crossref]
- Sinawang GW, Kusnanto K, Pratiwi IN. Systematic Review of Family Members in Improving the Quality of Life of People with T2DM. Jurnal Ners 2020;15:107-12. [Crossref]
- Zeidner M, Matthews G, Shemesh DO. Cognitive-Social Sources of Wellbeing: Differentiating the Roles of Coping Style, Social Support and Emotional Intelligence. J Happiness Stud 2016;17:2481-501. [Crossref]
- Pratiwi IN. Purwaningsih, Ramahwati S. The correlation between family support and quality of life in mothers with positive HIV in Surabaya. Indian Journal of Public Health Research and Development 2019;10:2703-7. [Crossref]
Cite this article as: Pratiwi IN, Nihayati HE, Santus R, Ramoo V, Nursalam N. Psychological impacts of the COVID-19 pandemic on nurses and coping strategies: a systematic review. J Public Health Emerg 2023;7:19.


