
Gender and racial disparity for hospital emergency service usage in USA: a quantitative analysis for various age groups during 2010–2017
Introduction
Health care disparity is an impious or iniquitous problem and has been a subject of healthcare policies and political debates for several decades. Measures, efforts and regulations have been evolving to try to mitigate disparity and allow fair resource allocation. Despite evidence and examples of disparity in the access to and provision of healthcare in various populations, there aren’t enough quantitative tools to measure disparity and to mitigate or eliminate it. There is a need to remove existing disparity due to socioeconomic forces which is not amplified by the users. It is important to determine how much emergency department (ED) overuse stems from individual factors like lack of insurance or primary referral sources and how much is due to systemic factors inherent in US healthcare. To fairly address the issue of unnecessary use of ED, it is prudent to assess if overuse is concentrated to a particular race or to a particular age group or a particular gender!
The goal of this analytical study was to examine and quantify disparity in racial and gender linked usage of ED services between 2010 and 2017 in USA and identify patterns for over or under use. The data for this study was compiled from publicly available sources based on the survey results of National Hospital Ambulatory Medical Care Survey (NHAMCS) (1,2) and works of various researchers identifying problems in healthcare delivery.
Soto et al. reviewed (3) the current literature on racial and gender disparities in critical care and the mechanisms underlying these disparities in the course of acute critical illness that showed such disparities as multifactorial and involve individual, community, and hospital-level factors responsible at several points spanning the duration of the acute critical illness.
Schrager et al. analyzed (4) the NHAMCS ED Subfile (2) between 2005 and 2014 and showed that black patients had 14% less chances of receiving diagnostic imaging in the ED compared to white patients. Natale et al. studied (5) 20 North American EDs between 2007–2010 for a total of 5,847 patients consisting of 54% white, 34% black and 12% Hispanics where black children had 20% lower chance of getting CT imaging for blunt abdominal trauma.
Shah et al. looked at (6) a total of 6,710 ED visits comprising 61% white, 20% black and 14% Hispanics. Compared to white patients, black patients and other races had 22–30% lower chance of getting pain analgesics. Work by Kressin et al. showed (7) that insurance instability and uncontrolled blood pressure went together for 44,000 adult ED visits during 2005–2013 in Massachusetts for age group of 21–64 and higher rates of uncontrolled blood pressure existed for blacks and Hispanics. In particular, uninsured black patients fared worst, while white and Hispanic patients with consistent public insurance fared best.
Interestingly, Crowe et al. looked at (8) the gender and racial composition of emergency medical technicians (EMTs) and paramedics and found that out of half a million that entered into the profession from 2008 to 2017 the proportion of females rose from 28% in 2008 to 35% in 2017 while black EMTs remained at 3–5% without any upward movement. From 1990 through 2017, Filut et al. observed (9) workplace discrimination even for advanced level healthcare providers—the physicians of color. Black physicians and women of color were discriminated through multiple sources; discrimination by patients was in the forms of refusal of care performed by black physicians.
Esper et al. analyzed (10) African American males that develop sepsis at a younger age needing ICU admission. Males developed more pulmonary infections resulting in 40% of sepsis cases while females developed sepsis from genitourinary sources that accounted for 10% of cases. African Americans in age groups <65 years developed more Gram-positive infections that were less responsive to therapy and led to severe illness and higher rates of acute organ failure as well as more invasive pneumococcal disease compared to whites.
Mohareb and co-authors noted (11) that HIV-infected individuals visited ED at 20% higher rates and consumed significantly more resources than the general population. Tabit et al. concluded (12) that without early consultation with a cardiologist in the ED low-socioeconomic urban patients for acute decompensated heart failure had over-utilized the ED (0.56 vs. 0.79, respectively) with increased re-hospitalization rate and health care cost. Pines et al. found (13) that during 2003–2005 staying back in ED longer after being admitted as in patient caused increased morbidity and mortality for black patients compared to whites admitted to ICU (6 vs. 5 hr) and to non-ICU beds (6.5 vs. 5.7 hr).
These national findings represented a baseline prior to full implementation of the 2010 Patient Protection under Affordable Care Act (ACA). It will be important to have sufficient quality control measures in ACA framework mitigating these disparities toward access and usage of ED services.
Work by Goyal et al. (14) revealed (racial and ethnic differences in antibiotic prescribing for acute respiratory tract infections. In the data from 7 pediatric emergency departments (PEDs) studied, compared to white children, black and Hispanic children received much less antibiotics for these infections. Dotson and co-authors investigated (15) in 38 hospitals the impact of race and insurance status on ED diagnostics and treatment among children with Crohn’s disease between 2007 and 2013 for age ≤21 years. White children from a higher median household income and private insurance (57% vs. 30% Medicaid) had a 40% higher chance for complete blood count and C-reactive protein/erythrocyte tests and 52% more chance of receiving antiemetics compared to Medicaid insured. Repeat visits due to complication or relapse was 33% for blacks and 22% for whites.
Hudgins et al. observed (16) that although only 6% pediatric patients presented to PEDs, the complexity of cases is higher compared to pediatric patients presenting to general EDs, and PEDs had greater rates of hospitalization (10% vs. 4%). The background presented on ED usage reveals complexity, and heterogeneity caused by different factors in rural and urban settings as well as in small vs. large EDs. Kahan and Morris found (17) that randomization of multiple centers (small and large) statistically performs better than fixed-effects approaches, i.e., drawing conclusions from limited gender or race based data even if such first-hand analyses offer actionable, local insights. Random center effects models lead to increased statistical power and precision when some centers have small number of patients, when there is an imbalance between treatments or the distribution of patients within centers. Note in our quantitative analysis using single patient normalization we have implemented such randomization to flatten the group heterogeneity.
New contribution
“Single user” normalization
This work focuses on understanding the factors that might have resulted in moderate to significant utilization differences in ED service by four groups as we have defined and are normalized to the habits and needs of a single user. Analysis of federal and state reports and peer-reviewed articles on ED usage and overuse from year 2010–2017 was undertaken followed by discussions with emergency department physicians and academic radiologists to gain insight and relevance for this work. Four groups as listed below were compared across all ages:
- All female ED users in US between 2010 and 2017;
- All male counterparts;
- All black ED users within the same period in US;
- All white counterparts.
Essentially this work analyzed usage patterns as if each group was made up of a single user irrespective of the location, demographics, training, resources or capabilities of ED allowing uniform analyses irrespective of the size and share of ED use by each group and normalizing local variation in ED care due to income, insurance or access.
Flattening of heterogeneity by randomization
This normalization to generate one user’s behavior during a single year flattened the seasonal heterogeneity like holiday patterns or flu season or back to school trends, for example. There are populations in USA that have a much greater fraction of 1-year-old than 14, while other regions may have many more 14-year-old than 1 making ED usage by the age group <15 across the whole USA quite heterogeneous. Single patient normalization is an example of randomization (17) that is better suited when an age group in certain race has smaller number of patients, as number of blacks age ≥75 years, compared to whites or when there is an imbalance between treatments, like in Crohn’s disease for Medicaid insured children mentioned above, Dotson et al. (15).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Study population
The study population consisted of all adult patients (n=202,480) with documented race, ethnicity and gender in the NHAMCS ED Subfile (1,2) between 2010 and 2017. NHAMCS is an annual nationally representative sample survey of visits to EDs; outpatient departments; and hospital-based and freestanding ambulatory surgical centers. NHAMCS-ED subfile we selected and analyzed was a consecutive 8-year long probability trend sample of ED visits in the US, collected by the Centers for Disease Control from a total of 3,055 hospitals and a statistically adequate responding EDs [65–82 patient records per ED each year out of 100 randomly asked, exception (*) in the year 2011, Table 1]. The characteristics of the data analyzed in this work are summarized below. In addition, works by other researchers were searched from literature using keywords like racial disparity, gender disparity, emergency services and ED usage and were analyzed for US primary emergency care disparities for the publication period from 2006–2020. Learning points from such prior works and our analysis have been included in the discussion section.
Table 1
| Year service utilized | Qualified hospitals total (n=3,055) | Participation rate (%) | Qualified ESA fulfilling criteria | Responding ESAs (%) fulfilling criteria | Patient records submitted (n=202,480) | Patient records/ESA |
|---|---|---|---|---|---|---|
| 2017 | 374 | 62.6 | 331 (240) | 72.5 | 16,709 | 70 |
| 2016 | 361 | 73.4 | 385 (271) | 70.4 | 19,467 | 72 |
| 2015 | 374 | 70.8 | 385 (291) | 77.8 | 21,061 | 72 |
| 2014 | 375 | 75.5 | 397 (319) | 80.4 | 23,844 | 75 |
| 2013 | 369 | 80.8 | 416 (339) | 81.5 | 24,777 | 73 |
| 2012 | 535 | 76.3 | 544 (454) | 83.5 | 29,453 | 65 |
| *2011 | 279 | 78.9 | 1,001 (847) | 84.6 | 32,233 | 38 |
| 2010 | 388 | 92.0 | 449 (427) | 95.1 | 34,936 | 82 |
*, A very low number of qualified hospitals and large number of ESAs in 2011 data may require re-assessment of original data collected in 2011. ED, emergency department; ESA, emergency department service area.
Inclusion criteria
Total number of qualified hospitals [3,055] surveyed with eligible ED’s ranged from 279–535 during 2010–2017 provided response rates of 62.6% to 92%. From those respondents 70.4–95.1% had met the criteria (of at least 50% of total patient visits during an arbitrarily chosen 4-week reporting period) by submitting a total of 202,480 records (yearly ranged from 16,709–34,936 records. The coding errors for the eligible records ranged from 0 to 1.5% during the 8-year analysis presented here. The low number of qualified hospitals in 2011 (*) data, almost doubling of emergency department service areas (ESAs) and a small number of patient records collected warrant further research.
Statistical analysis
ED use data was classified in four cohorts: two primary genders and two primary races as:
- All female ED users in US between 2010 and 2017;
- All male counterparts;
- All black ED users within the same period in US;
- All white counterparts.
Single user normalization model
Essentially this work analyzed usage patterns as if each group was made up of a single user irrespective of the population size allowing usage pattern to be compared without considering overall share of ED use by each group or including any variable related to income, health insurance or disease disparity. Each of these four groups were broken down to smaller, coherent age groups with similar usage; for example: all females age <15 vs. all males of age <15, all black patients (male and female) of age <15 vs. all white patients of age <15, and so on.
The total ED visits of each age group for each year were divided by the total US population of that age group to determine the ED usage fraction of a single person present in USA in each year (“single user normalized usage %”). Finally percentage differences of such usage fractions with relevant comparison groups were computed over the full US utilization by individual age groups.
Normalization steps
For example, the first entry (disparity %) in 2010 (Table 2) was computed as follows:
Table 2
| Age group, yr | ED service year | |||||||
|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 015 | 2016 | 2017 | |
| <15 | –42.4 | –50 | –26.8 | –39 | –28.8 | –35.6 | –31.6 | –35.8 |
| 15–24 | 19.6 | 37 | 17.6 | 25.6 | 20 | 21.2 | 27.1 | 23.7 |
| 25–44 | 16.6 | 40 | 9.5 | 15 | 11.7 | 16.6 | 10 | 13.5 |
| 45–64 | –8.3 | –4 | –10.8 | –11.5 | –10.2 | –9.3 | –5.5 | –8.1 |
| 65–74 | 3.2 | –14.7 | –10.1 | –2.8 | –4.3 | 0 | –8.6 | –0.8 |
| ≥75 | 23.3 | 16.6 | 24.4 | 31 | 26.2 | 14.3 | 17.7 | 24.8 |
ED, emergency department.
Single patient normalized disparity % in ED usage in 2010 = 100% × (total number of males & females in US of age <15 in 2010) × [(total female visits of age <15/total females in US of age <15) – (total male visits of age <15/total males in US of age <15)]/(total female visits of age <15 + total male visits of age <15 during 2010).
Results
Gender disparity
In Table 2 excess (+) or reduced (–) ED service usage (%) by female patients for various age groups is reported as compared to their male counterparts from 2010 to 2017 in the US.
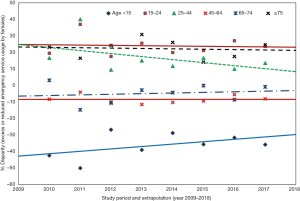
The following three gender disparity trends were observed across various age groups:
- Four age groups did not change the usage patterns over 8-year study period: age 15–24 (solid crimson) and those ages ≥75 (dashed black) showed females use ED approximately 25% more than males; females age 45–64 (solid red) and 65–74 (dotted blue) used ED same as males for these years.
- Girls compared to boys, age <15 have used (35–45% less) ED throughout this period.
- Young adult females, age 25–44, have used (15–25% more) ED service than adult male.
Race disparity
In Table 3 excess (+) or reduced (–) ED service usage (%) by black patients for various age groups is reported as compared to their white counterparts from 2010 to 2017 in US.
Table 3
| Age group, yr | ED service year | |||||||
|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| <15 | 12.4 | 0 | 15.6 | 9.2 | 22.5 | 11.4 | 24.4 | 16.8 |
| 15–24 | 16.7 | –4 | 13 | 14.7 | 26.6 | 13.8 | 16.3 | 18.8 |
| 25–44 | –25.1 | 8 | 6.2 | 15.3 | 8.5 | 14.5 | 11.9 | 13.7 |
| 45–64 | 4.5 | 11.5 | 7.5 | 4.7 | –5 | 3.6 | –11.2 | 3.1 |
| 65–74 | –38.6 | –7.1 | –40 | –44.4 | –55.2 | –51.5 | –38.3 | –49.6 |
| ≥75 | –60.3 | –53.5 | –80 | –97.1 | –106 | –88.4 | –76.2 | –111 |
ED, emergency department.
The following three racial disparity trends were observed across various age groups:
- Two black patient groups, age <15, solid blue and 15–24, crimson dashed, show modest, increase in the ED use, by 13–19% compared to the whites at the same ages.
- Blacks, age 25–44 (dashed green) showed a consistent, slightly more usage by about 10–14%. However, the usage for the two races for age 45–64 seems to be almost same.
- Importantly, after age 65 we see a dramatic and full reversal in usage: significantly reduced usage by blacks as early as 2010/2011: the disparity becomes increasingly prominent as blacks grow older. Elderly, age 65–74 (blue dashed line) and geriatric, age ≥75 years (black solid line), show 50–100% less ED use compared to whites by 2017.
Discussions
This work revealed large racial and gender differences in the use of ED services for most of the age groups in the nationally representative NHAMCS survey, between 2010 and 2017. We controlled for the contribution of population difference and singled out individual contributions from “herd behavior” in our analysis of ED utilization. The main advantage of the single user normalization (“methods” section) is its comparability without special accommodation to ED usage skewed by racial practices, age-related priorities, peer communication, geographic locations or ED size and specialty. For example, the differences in population, social communication and ED complexity for all the 1-year-old through all the 14-year-old were averaged out together by single user normalization for the age group of <15. We feel our single user representation model has a randomization advantage following the arguments of Kahan and Morris (17) in statistical strength.
On gender disparity across age groups
The results shown in Figure 1 emphasized that the need, usage and ED visit patterns were different for the two genders: for every 10 boys age <15 that visited the ED, only about 5–7 girls went to ED; for every 7 young males (age 15–44), 8–9 young females visited the ED while at middle to young old ages (45–75 yrs) both males and females used ED at a lower and almost at the same rate. At old geriatric age (≥75 yr), for every 4 male ED patients, the ED served 5 female patients. Carret et al. (18) observed that excessive ED use globally varied from 20% to 40% based on age and income variability. Female patients, patients without co-morbidities, without adequate insurance and those not referred to ED by a physician also showed excessive ED use.
On racial disparity across age groups
Racial disparity patterns also seem to be widespread: as shown in Figure 2, ED services were used very differently by blacks and whites although the disparity reversed at older age compared to the younger groups. In 2014, 4 black youths (age 15–24, orange line, +26.6%) made as many ED trips as 5 white youths while 4 geriatric black patients (age ≥75, green line, –106%) made only half as many trips to the ED as 4 white patients.
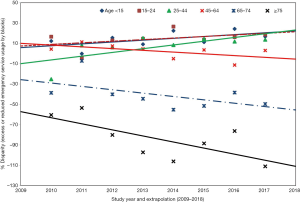
We may be able to draw one plausible cause for this: Rinaldi et al. observed (19) that non-physician healthcare providers as well as physicians practice of defensive medicine is mainly caused by fear of litigation; this includes both active and passive defensive medicine, such as over-investigation, over-treatment, and avoidance of high-risk patients. White elderly may have a greater litigation potential and less disease complexity than black patients of same age.
Kanzaria et al. surveyed (20) emergency medicine (EM) physicians about shared decision-making (SDM), a law under ACA, when physicians and patients collaboratively choose emergency management strategy from various reasonable options for patient-centered, high quality and effective emergency services. They found male and academic EM physicians tend to use less SDM for several perceived biases against SDM. Lack of black participation demonstrated by our analysis at middle and particularly at geriatric age raises the question if such patients were subjected to inadequate SDM at ED and had less choice compared to whites of same age.
There are several possible explanations for the differences observed in ED service utilization by race and gender, and the ultimate cause is likely a combination of factors. Given the nationally representative data source and the lack of clinical decision-making data, we cannot confirm whether the racial difference in ED use between black and white patients was the result of underuse by elderly black patients by choice or from economic and related constraints or overuse of ED services by elderly whites. The complexity or severity of disease burden or the awareness of it among whites could have been different and was not explored. It is unknown whether these racial differences observed had influenced health outcomes or whether the ED usage was clinically appropriate or followed any guideline recommendations.
Radiology department and inappropriate use of ED services
Of note, radiology service turnaround times and diagnostic accuracy intimately influence ED effectiveness and patient experience as well as quality of hospital care and readmissions. Jalal et al. (21,22) reviewed records during 2013–2017 from a tertiary ED environment to conclude that 24/7/365 radiology physician coverage significantly reduces turnaround time for diagnosis and thus disposition time in ED as corroborated by Hanna et al. (23). Additionally, Hanna et al. (24) also observed that in their patient population 60% of time a second imaging modality was applied without considering the results from the first as a demonstration of inefficient ED resource utilization. Quite frequently low-yield diagnostic imaging modalities for identifying the main issue have been used in ED causing prolonged turnaround time, unnecessary radiation exposure and added medical costs. Examples of such low-yield procedures are: shunt series radiography by Shuaib et al. (25), dedicated rib series from Shuaib et al. (26), sacrum and coccyx radiographs from works of Hanna et al. (27), routine use of facial CT from Shuaib et al. (28) as well as contrast enhanced head CT for non-traumatic neurological presentations in ED shown again by Shuaib et al. (29). Such inappropriate ED use causing prolonged turnaround time and treatment delays with added morbidity and costs when EDs are resource-starved might also cause disproportionate ED usage by specific populations.
Patient choice, role of urgent care and ACA
The growth and development of urgent care centers (UCC) in the context of overcrowded EDs could be partly responsible for somewhat preferred use of UCC by commercially insured. Declining competitiveness of ED services due to growing number of UCC for minor emergencies in major US cities may play a role in ED usage variation in recent years. Krause et al. reviewed (30) Truven Health MarketScan Research Databases of approximately 10M commercially insured UCC users in USA compared to approximately 93M primary care users during 2011–2015. They concluded that urgent care is meeting a need of convenience in spite of being costlier and is potentially replacing outpatient and emergency care for certain acute complaints. We feel since UCC requires upfront co-pay, several young black Americans may be preferably utilizing ED services while many young white Americans are choosing convenience over cost and hence UCC over ED. Coster et al. summarized (31) the reasons why some patients chose ED over UCC. They point to 24/7 access and confidence in acute ED primary care, higher urgency, greater anxiety, reassurance from emergency-based services, views of family, friends and healthcare professionals, convenient locations as well as having the full-service reputations as the primary reasons for choosing ED.
Gindi et al. found (32) the factors responsible for ED visits in 18% of their cohorts, aged 18–64 from 2013–2014. The visits were 77% due to seriousness of their presenting problems, 12% for emergencies occurring beyond outpatient office hours and 7% due to lack of insurance. Seriousness of the medical problems and lack of insurance were the primary reasons for the Medicaid and uninsured. Weinick et al. commented (33) on the implementation of health care reform under the ACA of 2010 and stressed that it is important to recognize that overall improvements in the US health care system might not automatically benefit all segments of the population equally. Based on our results we find the quality improvement efforts have not adequately removed various disparities nor created enough incentives for providers to serve minority patients in largely minority caring hospitals.
Study limitations
There are several limitations to the interpretation of the results we present in this investigation. As with other studies using the NHAMCS-ED survey, we recognize the inherent bias with using this data source, namely, heterogeneity in documentation from multi-center data pointed out by Vierron et al. (34) and missing responses. Most NHAMCS-ED data items have a nonresponse rate of approximately 5% to 10%. Patients missing race and ethnicity represented 6% of the study sample that is deemed acceptable for the current analysis.
However, despite this, the disparities in ED use by race and gender as demonstrated in this multiyear, nationally representative data analysis warrant further investigation due to potential bias from ignoring socioeconomic factors. Larger EDs tend to have longer wait times and a larger proportion of the black population, which may also contribute to the disparity of usage. This study did not adjust for the variables like insurance, family support and transportation available nor income or educational levels that could be confounding factors of preference, financial status and thus ED usage.
Therefore, we cannot specifically call these findings a true health care disparity. These are suggestive of but not conclusive enough to separate the differences that are due to structural, inherent weaknesses of healthcare from the ones that originate from individual choice and socioeconomic/educational make up of particular groups built over decades. The low number of qualified hospitals in 2011 (*) data (Table 1, “methods” section) while almost doubling of ESAs and a small number of patient records collected warrants scrutiny and was not addressed here.
Disparity models from past: Dahlgren and Whitehead rainbow model of determinants of health
The quality of health across all age groups depends on factors that are within as well as outside a patient’s control. Dahlgren and Whitehead model (1991/2007) ‘policy rainbow’ (35,36) describes multiple factors of influence on an individual’s health and focuses on the relationships between these factors, some of which are fixed (non-modifiable core factors: such as age, sex and genetics derived) and a set of individually modifiable factors: personal lifestyle, the physical and social, and broad socio-economic, cultural/environmental conditions. This “rainbow” model raises the awareness about the extent of influence of each of the factors on health, the feasibility of altering specific factors with specific actions that could influence additional linked factors. This widely recognized model allows one to construct hypotheses about the determinants of health as well as their interactions and influences on various health outcomes. In early 2000s in the US the relative impacts on early death from these determinants were approximately: 30% from genetic predispositions, 15% from social circumstances, 5% from environmental exposures, 40% from behavioral patterns and 10% from shortfalls in medical care (37).
However, the Dahlgren and Whitehead rainbow model is only applicable to US or other western countries with similar socioeconomic and environmental conditions and similar populations. Places with different population structure, different social conditions, may show a different result. For example, in a country where a pandemic or a civil war breaks out of control, health of the poor and middle class can deteriorate quite rapidly due to the general socio-economic and environmental disparity. In such a situation racial and gender inequality could result in suboptimal short- and long-term health among these classes. We believe such pandemics can skew the already heterogeneous database used in this work requiring further normalization than proposed here.
The 2003 WHO document ‘The Solid Facts’ points to such enormous differences in the social determinants of health and reviewed the causal relationships between social and environmental factors and poor health. Wilkinson and Marmot (37) have elicited the role of adequate policies in the presence of these basic differences. Both the works point out that poor social and economic circumstances affect health of those further down the social ladder at least twofold as well as early death compared to those near the top. The effects also run across the employment ladder similarly: lower ranking staff suffers much more disease and earlier death than higher ranking staff aggregated more with advancing age. These works seem to explain the significant disparity computed in the race disparity results of ours (Figure 2) for geriatric blacks i.e., a single black patient is twice less likely to take or get emergency service compared to a single white user of same age.
On behalf of the 2005 and 2010 WHO initiative, the Commission on Social Determinants of Health (CSDH), Solar and Irwin (38) drew the attention of governments, society, international organizations and donors to the health impacts of social determinants and highlighted various international and national causes of inequalities. It suggested practical ways of tackling these through creating better social conditions for vulnerable communities. According to CSDH, the social and environmental factors are at the root of most of the inequalities that result in both communicable and non-communicable diseases. However, the roles and failures of modern technological advances are not addressed in these documents. We may point out that genetic susceptibilities to disease for certain races or for a particular gender is ill understood and may produce devastating consequences for certain individuals as we are seeing with healthy life losses in COVID outbreak.
Also notice that the applicability of such models is limited to the identification and quantifiable analysis of disparity. Single user normalization approach in the current work normalizes the disparity trends with respect to group heterogeneity, geographic diversity and population size offering disparity quantification at the front end of policy and resource planning in regions that suffer from similar disparities. However, our work does not directly include or address the root causes of determinants of health while offer normalized quantification of trends that may help assess and apply Dahlgren and Whitehead rainbow model (35,36) where health determinants have heterogeneous groups of users.
Future implications
In this national multiyear study of patients in the NHAMCS-ED survey, we observed large racial and gender differences in ED services usage after separating the population by age, race and gender and by normalizing the population differences for various groups. In this work we were able to pinpoint how likely a single female or a single black patient utilized ED services as compared to a male or a white user during 2010–2017 irrespective of geographic location or affordability. Black patients were less likely to utilize or receive ED imaging than white patients past the middle age but not so at earlier ages. These observed differences warrant further investigation to determine whether this represents true racial or gender disparity in patient care. Future research will likely benefit from local examination of socioeconomic factors as well as from the positive effects of technology, manpower and medical advances available in radiology and ED services in recent years.
Our work offers empirical research with a normalization model that, we believe, stratifies the disparity comparison issues from a highly useful, although heterogeneous dataset. Given that complex data may continue to be collected from diverse sources this analysis could offer objective tools to analyze and influence policy and resource planning in countries that suffer from similar disparities. Given that the complexity of data sources will continue to prevail, simple and effective tools are needed to quantify and effectively reduce disparities in spite of the heterogeneity of service data that are used to make policies and resource planning. By normalizing the differential emergency services arising from individual centers in such a multi-center database (39) requires a normalizing tool as we have proposed here. Our analysis with a single user conversion is a part of the randomization (17) that allowed quantification of the disparities and flattened the local and seasonal effects of disease, crowding of inner cities, geographic disadvantages, friends and family habits, cultural bias, specialized ED quality and ED reputation etc. across USA including the age variation of users of this large database.
The ED services disparity seems to have been highlighted in the current COVID pandemic crisis. Recently, according to the Huffington Post News entry by Ignaczak and Hobbes (40) CDC has not released coronavirus data by race or gender. But city and state data indicate that COVID cases are heavily afflicting the black population. In Chicago, 23% of residents are black but accounted for 58% of COVID deaths. In Milwaukee, roughly 25% population is black suffering with approximately one-half of COVID cases. In Louisiana, 7 out of 10 COVID victims were black. Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said at a recent White House coronavirus task force briefing. “The things that get people into [intensive care]” and require them to be put on a ventilator—something that often leads to death—are the very factors, Fauci said, “that are, unfortunately, disproportionately prevalent in the African American population”.
Conclusions
This is the first comprehensive meta-analysis demonstrating racial and gender specific variation in the usage of emergency health care services that exist in USA and seem to be multifactorial and age specific. This study also found that the usage patterns from year to year were variable making prediction and resource planning a moving target. However, there were quantifiable trends of gender and racial disparities demonstrated by single user based randomization. This analysis may offer objective tools to analyze and influence policy and resource planning in regions that suffer from similar disparities. A current and stark example at the national level of such disparity is the disproportionate number of infections and deaths among blacks in current COVID Pandemic fallout in USA and deserves urgent attention. However, such pandemics can skew the already heterogeneous databases used in this work requiring further normalization than proposed here.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe-20-47). FK is the recipient of the AFMC-May Cohen Equity, Diversity and Gender Award (2020). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional ethical approval and individual informed consent were waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Centers for Disease Control and Prevention. NHAMCS micro-data file documentation, 2010-2017. Available online: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHAMCS
- National Center for Health Statistics. Survey Instruments. Available online: https://www.cdc.gov/nchs/ahcd/ahcd_survey_instruments.htm
- Soto GJ, Martin GS, Gong MN. Healthcare disparities in critical illness. Crit Care Med 2013;41:2784-93. [Crossref] [PubMed]
- Schrager JD, Patzer RE, Kim JJ, et al. Racial and ethnic differences in diagnostic imaging utilization during adult emergency department visits in the United States, 2005 to 2014. J Am Coll Radiol 2019;16:1036-45. [Crossref] [PubMed]
- Natale JE, Joseph JG, Rogers AJ, et al. Relationship of physician identified patient race and ethnicity to use of computed tomography in pediatric blunt torso trauma. Acad Emerg Med 2016;23:584-90. [Crossref] [PubMed]
- Shah AA, Zogg CS, Zafar SN, et al. Analgesic access for acute abdominal pain in the emergency department among racial/ethnic minority patients: a nationwide examination. Med Care 2015;53:1000-9. [Crossref] [PubMed]
- Kressin NR, Terrin N, Hanchate AD, et al. Is insurance instability associated with hypertension outcomes and does this vary by race/ethnicity? BMC Health Serv Res 2020;20:216. [Crossref] [PubMed]
- Crowe RP, Krebs W, Cash RE, et al. Females and minority racial/ethnic groups remain underrepresented in emergency medical services: a ten-year assessment, 2008-2017. Prehosp Emerg Care 2020;24:180-7. [Crossref] [PubMed]
- Filut A, Alvarez M, Carnes M. Discrimination toward physicians of color: a systematic review. J Natl Med Assoc 2020;112:117-40. [Crossref] [PubMed]
- Esper AM, Moss M, Lewis CA, et al. The role of infection and comorbidity: factors that influence disparities in sepsis. Crit Care Med 2006;34:2576-82. [Crossref] [PubMed]
- Mohareb AM, Rothman RE, Hsieh YH. Emergency department (ED) utilization by HIV-infected ED patients in the United States in 2009 and 2010 - a national estimation. HIV Med 2013;14:605-13. [Crossref] [PubMed]
- Tabit CE, Coplan MJ, Spencer KT, et al. Cardiology consultation in the emergency department reduces re-hospitalizations for low-socioeconomic patients with acute decompensated heart failure. Am J Med 2017;130:1112.e17-31. [Crossref] [PubMed]
- Pines JM, Localio AR, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med 2009;16:403-10. [Crossref] [PubMed]
- Goyal MK, Johnson TJ, Chamberlain JM, et al. Racial and ethnic differences in antibiotic use for viral illness in emergency departments. Pediatrics 2017;140:e20170203 [Crossref] [PubMed]
- Dotson JL, Kappelman MD, Bricker J, et al. Multicenter evaluation of emergency department treatment for children and adolescents with Crohn's disease according to race/ethnicity and insurance payor status. Inflamm Bowel Dis 2019;25:194-203. [Crossref] [PubMed]
- Hudgins JD, Monuteaux MC, Bourgeois FT, et al. Complexity and severity of pediatric patients treated at United States Emergency Departments. J Pediatr 2017;186:145-9.e1. [Crossref] [PubMed]
- Kahan BC, Morris TP. Analysis of multicentre trials with continuous outcomes: when and how should we account for centre effects? Stat Med 2013;32:1136-49. [Crossref] [PubMed]
- Carret ML, Fassa AC, Domingues MR. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad Saúde Pública 2009;25:7-28. [Crossref] [PubMed]
- Rinaldi C, D’Alleva A, Leigheb F, et al. Defensive practices among non-medical health professionals: an overview of the scientific literature. J Healthc Qual Res 2019;34:97-108. [Crossref] [PubMed]
- Kanzaria HK, Brook RH, Probst MA, et al. Emergency physician perceptions of shared decision-making. Acad Emerg Med 2015;22:399-405. [Crossref] [PubMed]
- Jalal S, Ouellette H, Ante Z, et al. Impact of 24/7/365 attending radiologist coverage on the turnaround time in an emergency and trauma radiology department. Can Assoc Radiol J 2020; [Epub ahead of print]. [Crossref]
- Jalal S, Lloyd ME, Khosa F, et al. Exploratory data analysis for pre and post 24/7/365 attending radiologist coverage support in an emergency department: fundamentals of data science. Emerg Radiol 2020;27:233-51. [Crossref] [PubMed]
- Hanna TN, Lamoureux C, Krupinski EA, et al. Effect of shift, schedule, and volume on interpretive accuracy: a retrospective analysis of 2.9 million radiologic examinations. Radiology 2018;287:205-12. [Crossref] [PubMed]
- Hanna TN, Shuaib W, Kerchberger JM, et al. Inefficient resource use for patients who receive both a chest radiograph and chest CT in a single emergency department visit. J Am Coll Radiol 2016;13:21-7. [Crossref] [PubMed]
- Shuaib W, Johnson JO, Pande V, et al. Ventriculoperitoneal shunt malfunction: cumulative effect of cost, radiation, and turnaround time on the patient and the health care system. AJR Am J Roentgenol 2014;202:13-7. [Crossref] [PubMed]
- Shuaib W, Vijayasarathi A, Tiwana MH, et al. The diagnostic utility of rib series in assessing rib fractures. Emerg Radiol 2014;21:159-64. [Crossref] [PubMed]
- Hanna TN, Sadiq M, Ditkofsky N, et al. Sacrum and coccyx radiographs have limited clinical impact in the emergency department. AJR Am J Roentgenol 2016;206:681-6. [Crossref] [PubMed]
- Shuaib W, Hashmi M, Vijayasarathi A, et al. The use of facial CT for the evaluation of a suspected simple dentoalveolar abscess in the emergency department. Clin Med Res 2015;13:112-6. [Crossref] [PubMed]
- Shuaib W, Tiwana MH, Chokshi FH, et al. Utility of CT head in the acute setting: value of contrast and non-contrast studies. Ir J Med Sci 2015;184:631-5. [Crossref] [PubMed]
- Krause TM, Ganduglia-Cazaban C, Piller LB, et al. Comparison of utilization of urgent care and primary care 2011-2015. Fam Med Care 2018. doi:
10.15761/FMC.1000102 . - Coster JE, Turner JK, Bradbury D, et al. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med 2017;24:1137-49. [Crossref] [PubMed]
- Gindi RM, Black LI, Cohen RA. Reasons for emergency room use among U.S. adults aged 18-64: National Health Interview Survey, 2013 and 2014. Natl Health Stat Report 2016;18:1-16. [PubMed]
- Weinick RM, Hasnain-Wynia R. Quality improvement efforts under health reform: how to ensure that they help reduce disparities—not increase them. Health Aff (Millwood) 2011;30:1837-43. [Crossref] [PubMed]
- Vierron E, Giraudeau B. Design effect in multicenter studies: gain or loss of power? BMC Med Res Methodol 2009;9:39. [Crossref] [PubMed]
- Dahlgren G, Whitehead M. 1991. Policies and strategies to promote social equity in health. Background document to WHO - Strategy paper for Europe. Arbetsrapport 2007:14, Institute for Futures Studies. Available online: https://ideas.repec.org/p/hhs/ifswps/2007_014.html
- Dahlgren G, Whitehead M. Levelling up (part 1& 2): a discussion paper on European strategies for tackling social inequities in health. Copenhagen: WHO Regional Office for Europe, 2006.
- Wilkinson R, Marmot M. editors. Social determinants of health: the solid facts. 2nd ed. Copenhagen: WHO Regional Office for Europe, 2003.
- Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). World Health Organization. 2010. Available online: https://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf
- Localio AR, Berlin JA, Ten Have TR, et al. Adjustments for center in multicenter studies: an overview. Ann Intern Med 2001;135:112-23. [Crossref] [PubMed]
- Ignaczak NM, Hobbes M. Black people are dying of COVID-19 at alarming rates. Here’s why. Huffington Post 2020. Available online: https://www.huffpost.com/entry/black-people-are-dying-of-covid-19-at-alarming-rates-heres-why_n_5e8cdb76c5b62459a930512a
Cite this article as: Sarkar SN, DeVito AF, Lespinasse E, Khosa F. Gender and racial disparity for hospital emergency service usage in USA: a quantitative analysis for various age groups during 2010–2017. J Public Health Emerg 2020;4:28.


