Pilot test results of a video-based HIV intervention for Chinese college students in the United States
Introduction
The United States (U.S.) hosts more of the world’s 4.5 million international students than any other country in the world (1). In 2015–2016, there were 1,043,839 international students studying in the U.S. (2). It is worth noting that students from China make up the largest group (34%) of international students in America's universities. Despite their significant large numbers in U.S. university campuses, very few culturally and linguistically appropriate HIV/sexually transmitted infection (STI) prevention programs have been developed and tested with this population. This pilot study assessed the efficacy of the translated Video Opportunities for Innovative Condom Education and Safer Sex (VOICES) intervention on the transtheoretical model (TTM) stages of change, self-efficacy in using condoms, perceived benefits and barriers to condom use, and knowledge of HIV/AIDS among Chinese college students studying at a local university in the United States.
Background
According to the latest estimates, 510,000 people in China were living with HIV/AIDS in China in 2013 and 501,000 reported cases of people living with HIV/AIDS at the end of 2014 (3). While male and female condoms used consistently and correctly may significantly lower the risk of transmission of HIV and other STIs (4), research evaluating condom use among Chinese college students in China, Taiwan, and the USA revealed that nearly one third consistently used condoms, and a wide range of study participants (10–75%) reported never using condoms (5-10). Other investigations of Chinese students indicated that sex education should be strengthened (4,11) and that a number of students had limited or inaccurate knowledge in regards to HIV and STIs. In addition, one fifth of Chinese college students were not aware that using condoms reduces the risk of HIV/STIs transmission (9,11,12). The lack of comprehensive knowledge about HIV/STIs among Chinese college students increases the vulnerability to HIV/STIs. Moreover, the potential impacts of studying abroad on Chinese students may further increase their vulnerability to HIV infections under some conditions such as problematic drinking.
VOICES is classified as a best-evidence program through the CDC efficacy review process. It was originally designed to promote condom use and enhance skills to negotiate condom use with their partners that targeted adult heterosexual African-American and Latino populations at risk for HIV/STDs (13). Intervention materials are available in English and Spanish languages. The implementation of the VOICES has been proved to decrease STI incidence, enhance condom use intentions and self-efficacy, and improve HIV/STIs knowledge in different ethnic groups in the U.S. (14-17). Considering the learning preference of receiving HIV/STI information from video watching in Chinese college students, this video- and evidence-based was chosen for this study (9,18,19). Furthermore, the VOICES program is brief and simple to implement.
Conceptual framework
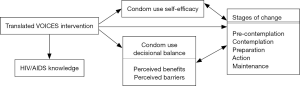
The conceptual framework (Figure 1) is a modification of the TTM. The TTM suggests that people differ in their readiness to engage in a particular behavior and incorporates several core concepts, stages of change, self-efficacy, and decisional balance (20). Individuals adopting a healthier behavior such as condom use progress through five stages of change (ordered from early to late in the change process): pre-contemplation, contemplation, preparation, action, and maintenance. Self-efficacy is the level of self-confidence to perform various tasks (21). Decisional balance is defined as weighing the perceived benefits against the perceived barriers of engaging in a health behavior (20). As posited by the TTM, the interrelations of these constructs in regards to condom use are (I) individuals report the lowest levels of self-efficacy in the precontemplation stage and the self-efficacy level can be expected to rise across the stages of change; and (II) individuals in precontemplation elevate the negative aspects of using condoms as higher than the perceived benefits of their use and that the relation between perceived benefits and barriers would be reversed for individuals in the maintenance stage. TTM studies assessing condom use support these hypothesized relationships between these constructs (22-25). This study employed the TTM stages of change approach that allows for identifying variables associated with the VOICES programs. Nurses play a vital role in the development and implementation of culturally sensitive HIV programs for this vulnerable population to reduce HIV-related health disparities. This study provides important insights for public health professionals to plan culturally relevant, and theory- and evidence-based HIV interventions that target the particular needs of Chinese college students in cost-effective ways. Our study evaluated the efficiency of the translated VOICES program on the TTM stages of change, condom use self-efficacy, perceived benefits and barriers to condom use, and HIV/AIDS knowledge among Chinese college students studying in a U.S. university. It is hypothesized that:
- Students will demonstrate a significant increase in the proportion in achieving the later TTM stage of change on the posttest than pretest;
- Students will demonstrate a significantly higher level of condom use self-efficacy on the posttest than pretest;
- Students will perceive significantly more benefits of and fewer barriers to regular condom use on the posttest than pretest;
- Students will demonstrate a significantly higher level of HIV/AIDS knowledge on the posttest than pretest.
Methods
Design
A quasi-experiment design with a single group pre-test/post-test was conducted in Chinese. The Institutional Review Board from investigator’s university approved this study.
Setting and sample
Study participants were obtained from a convenience sample of Chinese students studying in a U.S. university. A research assistant disseminated the invitation and information letter via email to Chinese students at university. Students were eligible for inclusion if they: (I) self-identified as Chinese; (II) had never been married; (III) had the ability to effectively communicate and read in Chinese; and (IV) were aged 18 years old or older in non-health related majors. Power analysis was conducted to estimate the necessary sample size. Assuming a 5% significance level 5%, 80% power, and a moderate effect size 0.4 for paired t-tests, the required sample size was 51. The final study population comprised of 67 students.
Instruments
The participants completed surveys in Chinese by prior to and immediately after the intervention (Figure 2). The self-administered survey questionnaire was divided into five sections as follows: (I) demographic information; (II) sexual history and condom use information (26); (III) condom use self-efficacy (27); (IV) condom use decisional balance (26); and (V) international AIDS questionnaire (28). The demographic information collected participants’ data including age, gender, level of study, perceived health status, and ever receiving sex education classes.
Sexual history and condom use information
The sexual history assessed if the participants had ever engaged in any sexual activities while the condom use survey used a five-item algorithm to measure the stage of change for condom use as defined by TTM (26). Participants were categorized into one of the five TTM stages on the basis of questions about the frequency and duration of their condom use and intention to use condoms every time they have vaginal, oral, or anal intercourse in the future.
Condom use self-efficacy scale
This scale contains 10 items to assess the strength of individuals’ confidence in their ability to use condoms in different circumstances (27). The items were rated on a 5-point Likert scale, ranging from 1= not at all confident to 5= very confident, with higher scores indicating greater confidence. In this study, the Cronbach’s alpha score was 0.96.
Condom use decisional balance scale
The scale consisting of a five-item perceived benefit scale and a five-item perceived barrier scale that assessed one’s perceived benefits and barriers of condom use on a 5-point Likert scale with 1 (not important) and 5 (extremely important) (26). Participants were asked to rate the importance of each of the items to use condoms. Higher scores represented greater perceived benefits and barriers. The Cronbach’s alphas were 0.88 and 0.84 for the Benefits and Barriers subscales, respectively.
International AIDS Questionnaire-Chinese Version (IAQ-C)
The IAQ-C developed by Davis and colleagues (28) included 13 items to measure HIV/AIDS-related knowledge. Each item was rated on a 5-point Likert scale (1= strongly agree to 5= strongly disagree), higher scores representing more accurate knowledge on HIV/AIDS. The Cronbach’s coefficient was 0.71.
Intervention
We obtained permission to use the VOICES program and translate materials into Chinese. The final translated version of the VOICES was developed based on the feedback provided by 20 Chinese college students. The intervention comprised four sessions facilitated by the first author (Figure 2). Before starting the session, the investigator outlined the ground rules (e.g., using no last names, everything said in the group stays in the group, recognizing everyone’s experiences and suggestions as valuable, not making fun of or judging others) for group discussion. During the small-group discussion and condom feature presentation, the investigator (I) used the situations depicted in the video to launch the discussion; (II) asked participants to role-play condom negotiation strategies; (III) asked participants what they would do if partners might not want to use condoms; (IV) introduced different types of condoms; (V) demonstrated how to put on and remove condoms; and (VI) presented a list of various local resources (13). Participants were asked to complete questionnaires before and immediately following intervention. At the end of the intervention, a $10 gift card was offered to each.
Data analysis
SAS version 9.4 for Windows was used to analyze data. Descriptive statistics were performed to describe the demographic data, condom use intentions, self-efficacy, perceived benefits and barriers to condom use, and HIV/AIDS knowledge. McNemar’s test was used to detect the difference in proportion of condom use intention between the pretest and posttest. Paired t-tests were performed to evaluate the differences in the level of self-efficacy, perceived benefits and barriers, and HIV/AIDS knowledge between the pretest and posttest. The significance threshold was set at P<0.05.
Results
Participant characteristics
Sixty-seven participants were enrolled in the study (Figure 2). Of the 67 participants, the mean age of the participants was 25.6 years, ranging from 20 to 38 (SD =3.73) years. Most of the participants were males (55.2%, n=37), graduate students (53.7%, n=36), and in good or excellent health condition (86.6%, n=58). Approximately half (49.2%, n=33) of individuals had prior sex education.
Difference in the proportion of intention to condom use stages and levels of self-efficacy, perceived benefits and barriers, and HIV/AIDS knowledge
On the basis of participants’ responses to the stage of condom use on the pretest, 22.4% (n=15) of the participants identified themselves in the precontemplation stage, 20.9% (n=14) in the contemplation stage, 20.9% (n=14) in the preparation stage, 14.9% (n=10) in the action stage, and 20.9% (n=14) in the maintenance stage. Because of the relatively small number of participants in the each stage and individuals in the contemplation, preparation, action, and maintenance stages intended to use condoms, the data in these four stages were combined into a single category (Table 1). McNemar’s test showed that students had a significant increase in the proportion in intention to use condom stages on the posttest than on the pretest (95.2% vs. 77.6%, P=0.002).
Table 1
| Intention to use condoms | Pretest, n (%) | Posttest, n (%) | P |
|---|---|---|---|
| Precontemplation (no intention to use condoms) | 15 (22.4) | 3 (4.8) | – |
| Intended to use condoms in the future1 | 52 (77.6) | 64 (95.2) | 0.002 |
1, The contemplation, preparation, action, and maintenance stages were combined into a single category.
As seen in Table 2, the posttest scores were significantly higher scores than pretest in the followings: (I) condom use self-efficacy; (II) perceived benefits; and (III) HIV/AIDS knowledge. The participants reported significantly lower scores on the posttest than pretest in perceived barriers to condom use.
Table 2
| Variables | Pretest, M (SD) | Posttest, M (SD) | t | P |
|---|---|---|---|---|
| Condom use self-efficacy | 3.78 (0.91) | 4.29 (0.84) | 5.38 | <0.0001 |
| Perceived benefits | 4.27 (0.63) | 4.51 (0.65) | 3.52 | 0.008 |
| Perceived barriers | 2.77 (0.91) | 2.36 (1.01) | −2.94 | 0.004 |
| HIV/AIDS knowledge | 4.08 (0.55) | 4.46 (0.52) | 6.39 | <0.0001 |
SD, standard deviation.
Discussion
This is the first study conducted in the U.S. examining the implementation of a translated VOICES intervention to reduce HIV/STIs in Chinese college students. Consistent with previous VOICES studies, the study results reveal that this translated program can increase peoples’ intentions and self-efficacy to use condoms, and improve HIV/STIs knowledge (14-17). These results suggest that VOICES has the potential to produce positive changes for preventing HIV among different populations and settings. Moreover, the consistent findings may be attributable to the fact that each facilitator received the same preparation and materials through CDC sponsored Diffusion of Effective Behavioral Interventions training (14).
The TTM was effective in predicting condom use intention among participants. As suggested by the TTM, moving towards the later stages of change involves increasing self-efficacy and perceived benefits, and decreasing perceived barriers. After watching the translated VOICES video and participating in a group discussion, the participants demonstrated a progression from the precontemplation to the more advanced stage of the TTM. These results support previous TTM work that shows people changing behaviors progress through several stages of change (22-25). The use of the TTM identified variables associated with the VOICES has implications for Chinese populations and will need additional investigation.
An increase in the participants HIV/AIDS knowledge was achieved after the intervention, which is similar to past research demonstrating the effectiveness of the VOICES in increasing HIV/AIDS knowledge (15-17). These results are not surprising, given that VOICES was intended to increase HIV/STI knowledge and intervention involves messages about condom and HIV/STI prevention.
Limitations
The study only included Chinese students at a single U.S. university, thus limiting the generalizability of the results to other universities. This study was a quasi-experimental design that lacked randomization. The results can be influenced by the pretest-posttest design. Finally, the use of a translated VOICES targeted toward Hispanic viewers may have affected the effectiveness of the intervention although significant results were obtained in this study. This point highlights the importance of in identifying culturally appropriate factors for the Chinese student population and developing targeted video interventions in the future.
Conclusions
The use of the translated VOICES demonstrates the effectiveness in Chinese students. Universities with Chinese students may consider incorporating this intervention during orientation at the university. The development of linguistically- and culturally-appropriate intervention to educate a vulnerable population in the U.S. about condom use and HIV/AIDS can help achieve the U.S. Healthy People 2020 objectives of increasing the proportion of sexually active persons who use condoms and reduce the rate of HIV/STI transmission among adolescents and adults (29). Finally, the study results provide insight into the constructs of the TTM in predicting condom use. This has implications for health professionals to use as a basis for the design of HIV programs for Chinese students.
Acknowledgments
Funding: This study was supported by the American Nurses Foundation (ANF 1830).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe.2017.11.01). WY serves as an unpaid editorial board member of Journal of Public Health and Emergency from May 2017 to Apr 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Permission to conduct the study was obtained from the University Institutional Review Board (No. IRB S10/11-097) prior to the start of this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- U.S. Embassy and Consulate in Vietnam. Open Doors Report: Vietnam is Sixth Leading Source of Foreign Students in the United States. Available online: https://vn.usembassy.gov/20161115-press-release-open-doors-report-vietnam-sixth-leading-source-foreign-students-united-states/
- Institute of International Education. Opendoors 2016 “Fast Facts”: International Students in the U.S. Available online: https://www.iie.org/Research-and-Insights/Open-Doors/Data/International-Students/Enrollment/Enrollment-Trends
- Joint United Nations Programme on HIV/AIDS (UNAIDS). 2015 China AIDS Response Progress Report. Available online: http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf
- U.S. Department of Health and Human Services (2014). Using Condoms. Available online: https://www.aids.gov/hiv-aids-basics/prevention/reduce-your-risk/using-condoms/
- Chen M, Liao Y, Liu J, et al. Comparison of sexual knowledge, attitude, and behavior between female Chinese college students from urban areas and rural areas: A hidden challenge for HIV/AIDS control in China. BioMed Research International 2016;2016:8175921 [PubMed]
- Liu Z, Wei P, Huang M, et al. Determinants of consistent condom use among college students in China: Application of the Information-Motivation-Behavior Skills (IMB) model. PLoS One 2014;9:e108976 [Crossref] [PubMed]
- Tung WC, Cook MD, Lu M. Sexual behavior, stages of condom use, and self-efficacy in college students in Taiwan. AIDS Care 2011;23:113-20. [Crossref] [PubMed]
- Tung WC, Cook MD, Lu M. Sexual behavior, decisional balance, and self-efficacy among Chinese college students in the U.S. J Am Coll Health 2012;60:367-73. [Crossref] [PubMed]
- Tung WC, Hu J, Efird JT, et al. HIV-related knowledge, attitudes, and behaviors among college students in China. Health Education Journal 2012;71:606-16. [Crossref]
- Wang YC. Individual, interpersonal, and community predictors of consistent condom use among Taiwanese university students. AIDS Care 2016;28:354-8. [Crossref] [PubMed]
- Sun X, Liu X, Shi Y, et al. Determinants of risky sexual behavior and condom use among college students in China. AIDS Care 2013;25:775-83. [Crossref] [PubMed]
- Chen H, Zhang L, Han Y, et al. HIV/AIDS knowledge, contraceptive knowledge, and condom use among unmarried youth in China. AIDS Care 2012;24:1550-8. [Crossref] [PubMed]
- Center for Disease Control and Prevention. VOICES/VOCES: Video Opportunities for Innovative Condom Education and Safer Sex. Available online: https://www.cdc.gov/hiv/pdf/research/interventionresearch/compendium/cdc-hiv-voices_voces_best_rr.pdf
- Fisher HH, Patel-Larson A, Green K, et al. Evaluation of an HIV prevention intervention for African Americans and hispanics: Findings from the VOICES/VOCES community-based organization behavioral outcomes project. AIDS Behav 2011;15:1691-706. [Crossref] [PubMed]
- Neumann MS, O’Donnell L, Doval AS, et al. Effectiveness of the VOICES/VOCES sexually transmitted disease/human immunodeficiency virus prevention intervention when administered by health department staff: Does it work in the “real world”? Sex Transm Dis 2011;38:133-9. [Crossref] [PubMed]
- O’Donnell CR, O’Donnell L, San Doval A, et al. Reductions in STD infections subsequent to an STD clinic visit. Using video-based patient education to supplement provider interactions. Sex Transm Dis 1998;25:161-8. [Crossref] [PubMed]
- O’Donnell LN, San Doval A, Duran R, et al. Video-based sexually transmitted disease patient education: Its impact on condom acquisition. Am J Public Health 1995;85:817-22. [Crossref] [PubMed]
- Tung WC, Ding K, Farmer S. Knowledge, attitudes, and behaviors related to HIV and AIDS among college students in Taiwan. J Assoc Nurses AIDS Care 2008;19:397-408. [Crossref] [PubMed]
- Tung WC, Lu M, Cook DM. HIV/AIDS knowledge and attitudes among Chinese college students in the US. J Immigr Minor Health 2013;15:788-95. [Crossref] [PubMed]
- Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Viswanath K, editors. Health behaviour and health education: Theory, research, and practice. San Francisco: Jossy-Bass, 2015:125-48.
- Bandura A. Self-efficacy: The exercise of control. New York: Freeman, 1997.
- Grossman C, Hadley W, Brown LK, et al. Adolescent sexual risk: factors predicting condom use across the stages of change. AIDS Behav 2008;12:913-22. [Crossref] [PubMed]
- Gullette DL, Wright PB, Booth BM, et al. Stages of change, decisional balance, and self-efficacy in condom use among rural African-American stimulant users. J Assoc Nurses AIDS Care 2009;20:428-41. [Crossref] [PubMed]
- Kwon YM, Yeun EJ, Kim HY, et al. Application of the transtheoretical model to identify aspects influencing condom use among Korean college students. West J Nurs Res 2008;30:991-1004. [Crossref] [PubMed]
- Pallonen UE, Timpson SC, Williams ML, et al. Stages of consistent condom use, partner intimacy, condom use attitude, and self-efficacy in African-American crack cocaine users. Arch Sex Behav 2009;38:149-58. [Crossref] [PubMed]
- Grimley DM, Prochaska JO, Velicer WF, et al. Contraceptive and condom use adoption and maintenance: a stage paradigm approach. Health Educ Q 1995;22:20-35. [Crossref] [PubMed]
- Redding CA, Rossi JS. Testing a model of situational self-efficacy for safer sex among college students: Stage of change and gender-based differences. Psychol Health 1999;14:467-86. [Crossref]
- Davis C, Tang CSK, Chan SFF, et al. The development and validation of the International AIDS Questionnaire-Chinese Version (IAQ-C). Educ Psychol Meas 1999;59:481-91. [Crossref]
- U.S. Department of Health and Human Services (2016). Healthy People 2020 Objectives: HIV. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/hiv/objectives
Cite this article as: Tung WC, Lu M, Rull R, Yang W. Pilot test results of a video-based HIV intervention for Chinese college students in the United States. J Public Health Emerg 2017;1:84.