Requirements for health prevention and control for COVID-19 during radiological diagnosis in Jiangsu Province
Introduction
A cluster of pneumonia cases with an unknown cause occurred in Wuhan, Hubei Province starting on December 2019, Chinese Center for Disease Control and Prevention (China CDC) immediately conducted epidemiological and etiological investigations into the disease. The first complete genome of the novel β genus coronaviruses (2019-nCoVs) was identified in samples of bronchoalveolar lavage fluid (BALF) from a patient from Wuhan, the virus has been designated as SARS-CoV-2, and the disease has been named the 2019 novel coronavirus disease (COVID-19) by the World Health Organization (WHO) (1). With the spread of the disease, COVID-19 was included in category B infectious diseases, and management of category A infectious diseases was adopted. According to the Prevention and Control Program of novel coronavirus pneumonia (version 4), SARS-CoV-2 is a novel β genus coronaviruses (2). The virus is sensitive to ultraviolet rays and heat. It can be effectively inactivated by heating to 56 °C for 30 minutes or using organic solvents such as ether, 75% ethanol, chlorine-containing disinfectant, peracetic acid and chloroform. Confirmed cases and asymptomatic infection may be the source of infection. The main route of transmission is through respiratory droplets and contact, and population aggregation predisposes to infection.
According to the Diagnosis and treatment of novel coronavirus pneumonia (trial version 5), the imaging characteristics of pneumonia is one of the clinical manifestations of suspected cases in Hubei Province (3). X-ray digital radiography (DR) and X-ray computed tomography (CT) using multiple uses such as fixed places, mobile, and mobile cabin played important roles in the diagnosis of the COVID-19. During the treatment process multiple radiographic examinations would be taken, and CT is gradually replacing DR to play an increasingly important role.
During radiological diagnosis of COVID-19, close contact between X-ray diagnostic staff and fever patients, suspected or confirmed cases brings risks of ionizing radiation hazards and nosocomial infections. Guidelines for the prevention and control of novel coronavirus pneumonia infections in medical institutions. (version 1) specify that medical institutions should strengthen management of key departments as well as patient isolation, disinfection and protection, nosocomial infection control (4). However, the key departments in the guidelines do not involve the inspection and medical imaging departments, so it is necessary to establish and improve the nosocomial infection control system to make up for these deficiencies. Jiangsu Provincial Center for Disease Control and Prevention (Jiangsu CDC) has compiled guidelines for infection prevention and control in X-ray imaging diagnosis to standardize nosocomial infection control and guide medical institutions in the province to carry out health protection in X-ray imaging diagnosis of the pneumonia (5).
Methods
Analysis of hazard factors in emergency treatment
X-ray imaging diagnosis involved in the diagnosis and treatment of the novel coronavirus pneumonia mainly includes chest DR and CT. Chest DR serves as an important screening tool in a medical environment with high incidence of the COVID-19 but limited resources. On the other hand, the chest CT scan is more sensitive to early or mild pneumonia, and it has an obvious follow-up effect during the treatment of the disease. It is an important method for early detection of the COVID-19 (6,7).
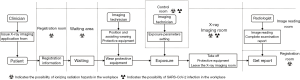
For most X-ray imaging diagnosis procedures, the following process is generally used after the clinician issues an X-ray imaging examination application form (Figure 1).
During mobile radiography, the radiologist and the patient operate in the same room, and the radiographic diagnosis in the fixed place and mobile cabin are operated in the compartment. Analysis of ionizing radiation hazards during X-ray imaging diagnosis point out that radiologists may be exposed to scattered radiation from DR or CT in the control room or operating position, and patients are exposed to the useful radiation or leakage radiation. It has been reported that the Hubei Provincial Center for Disease Control and Prevention have carried out radiation protection monitoring on the CT imaging rooms of Huoshenshan Hospital, Leishenshan Hospital and the Wuhan Third Hospital, and have taken temporary protective measures against the problems found (8).
Based on the prevention and control situation of the novel coronavirus pneumonia, the possible infection factors during the diagnosis of X-ray imaging were also analyzed. Sources of infection are suspected or confirmed patients, asymptomatic infections, and places or items contaminated by the virus such as the X-ray imaging room, diagnostic equipment and protective equipment. The main routes of infection are respiratory droplets and contact transmission to X-ray imaging diagnostic staff and non-viral infection patients during information registration and receipt of inspection reports, wearing protective equipment in the X-ray imaging room, and receiving the positioning of the imaging technicians. At present, some hospitals have found that several radiology staff are infected with the SARS-CoV-2.
Therefore, it is necessary to carry out protection and disinfection for personnel, places, equipment and articles related to radiological diagnosis of COVID-19, and to carry out monitoring of hazard factors and risk assessment to ensure the orderly radiological diagnosis of the pneumonia.
Results
Based on the analysis of the hazard factors in the X-ray imaging diagnosis, Guidelines for the prevention and control of X-ray imaging diagnosis of new coronary pneumonia in Jiangsu medical institutions (trial) has been compiled by Jiangsu CDC. This guideline clarifies the basic requirements for infection management and radiation protection during radiological diagnosis, it also clarifies the requirements for staff protection, personnel disinfection, site disinfection as well as client protection and disinfection.
Conclusions
Basic requirements
Protection against ionizing radiation: According to Basic standards for protection against ionizing radiation and the safety of radiation sources (GB18871-2002) (9) and Requirements for radiological protection in medical X-ray diagnosis (GBZ130-2013) (10), optimization of radiation protection and safety should be implemented to ensure that the annual effective dose of staff meets the management target requirements of medical institutions. Make sure that the dose to patients is as low as possible while ensuring adequate imaging diagnostic information is available. X-ray diagnostic equipment's protective performance, X-ray imaging room protective facilities and operation of protection and safety should meet the requirements of GBZ130-2013.
Infection control: Medical institutions should incorporate radiology into hospital infection management, implement responsibilities, carry out supervision and inspection, and health professionals for X-ray imaging diagnosis should undergo infection management training. Medical institutions shall designate a dedicated X-ray imaging diagnosis work area and configure a dedicated DR and/or CT for X-ray imaging diagnosis of patients infected by the novel coronavirus. Separate the work area for image diagnosis as far as possible from other areas, and stop using central air conditioning equipment. The equipment control room should be equipped with necessary disinfection supplies and tools to facilitate health professionals to carry out disinfection in time.
Personal protection and disinfection requirements
Personal protection requirements should be provided when using mobile X-ray machines for bedside radiography (lead rubber apron, lead rubber hat, lead rubber neck cover, lead rubber gloves, lead protective glasses, equipped with lead protective screen, etc.). Strengthen the management of individual monitoring of occupational external exposure for radiation workers. The dosimeter should be equipped on the left chest of the inner coverall or the collar corresponding to the collarbone, not on the outside of medical disposable protective clothing. Pay attention to the cleaning and disinfection of the dosimeters during the wearing, recycling, and monitoring.
Health professionals and cleaning and disinfection personnel who register in the designated work area or enter the X-ray imaging room to directly contact the patient should follow the requirements of the staff of the isolation ward and the medical observation site. It is recommended to wear work clothes, disposable work caps, disposable gloves, medical disposable protective clothing, medical protective masks (N95 or better), protective screens or goggles, work shoes or rubber boots, waterproof boot covers, etc. Disinfection personnel should take personal protection when preparing and using chemical disinfectants.
Staff disinfection measures include hand disinfection, skin disinfection and disinfection when wearing or taking off protective clothing. As hand hygiene measures for health professionals, when there is obvious pollution on hands, 70% to 75% ethanol or 70% ethanol washing-free hand sanitizing gel, or other effective alcohol-containing quick-drying hand sanitizers can be used, when there are visible pollutants, hand sanitizer should be used under running water, hand disinfection should be carried out after drying with tissue.
When the skin of health professionals is contaminated, the pollutants should be immediately removed, and disinfected with a disposable absorbent material with 0.5% iodophor or hydrogen peroxide disinfectant for more than 3 minutes, then washed with water. Mucosa should be rinsed with a large amount of normal saline or 0.05% iodophor.
Health professionals should minimize contact with contaminated surfaces when removing protective clothing. The non-disposable items such as the protective goggles and rubber boots that have been removed should be directly immersed in a container filled with disinfectant solution; the disposable items should be placed in a yellow medical waste collection bag for centralized disposal as medical waste. Health professionals should perform hand disinfection at each step when removing protective equipment, and disinfect hands again after all protective equipment is removed.
Patients protection and disinfection requirements
To ensure the optimization of medical exposure of the patients, more protective equipment should be equipped (such as lead rubber gonad protective apron or square scarf, lead rubber hat, lead rubber neck cover, lead protective screen and equipments for fixing the special position of patients), and inspection parameters of X-ray imaging diagnostic should also be optimized. Patients must wear masks and gloves for X-ray imaging. The bed of diagnosis equipment must be laid with disposable sheets which should be replaced after each diagnosis. After inspection, the disposable supplies should be disposed as infectious medical waste. Reusable personal protective equipment should be disinfected with 75% ethanol in time. Adopt radioprotection measures for nearby patients during bedside radiography using mobile X-ray machines in isolation wards. After the radiography, the mobile X-ray machine and lead rubber protective clothing should be disinfected with 75% ethanol.
Workplace disinfection requirements
The X-ray image diagnosis X-ray imaging room should be ventilated 2 to 3 times a day for more than 30min each time. In the working state, air disinfection can be performed by natural ventilation, powered ventilation (non-central air conditioning system) or circulating air disinfection machine. In the unmanned state, UV germicidal lamp or mobile UV lamp should be installed evenly in areas where patients stay longer, such as X-ray imaging rooms and waiting areas until meet the 1.5 W/m3 standard, UV disinfection should be carried out 1 or 2 times a day, more than 1 hour each time. The floor and walls of the X-ray imaging room, X-ray diagnostic equipment surface, related diagnostic supplies and the air indoor should be disinfected after the daily work.
According to Regulation of disinfection technique in healthcare settings (WS/T367-2012), in the absence of visible contaminants, the surface of the object (non-precious instrument surface) and ground should be wiped with 400–700 mg/L of available chlorine (11). After 30 minutes, the surface should be wiped with clean water. The surface of X-ray imaging diagnostic equipment should be wiped and disinfected with 75% ethanol. In the presence of visible contaminants, a small amount of them can be carefully removed by disposable absorbent materials (such as gauze, rags, etc.) with 5,000–10,000 mg/L of chlorine-containing disinfectant (or disinfection wipes/dry towels capable of achieving high levels of disinfection). After removing the contaminants, the surface should be wiped and disinfected with 1,000 mg/L effective chlorine disinfectant. After 30 minutes, the surface should be wiped with clean water.
The patient's vomit or other large amount of pollutants should be cleaned and disinfected in time during X-ray diagnosis. The pollutants should be covered completely with disinfecting powder or bleaching powder containing water-absorbing ingredients, or be covered completely with secondary water-absorbing material which is poured a sufficient amount of 5,000–10,000 mg/L chlorine-containing disinfectant. After at least 30 minutes, the pollutants should be carefully removed. During the cleaning process, contact with pollutants must be avoided, and the cleaned up pollutants should be disposed as medical waste centrally.
Health monitoring requirements
During the epidemic of COVID-19, the occupational exposure monitoring and evaluation of radiology staff should be strengthened, and the surface monitoring of radiology equipment and articles, radiological protection in the workplace and air sample monitoring should be carried out. As for radiological protection, due to the large-scale use of mobile cabin CT and mobile DR, radiological protection monitoring in hospitals should be strengthened to ensure medical quality and medical safety. On the premise of guaranteeing the health rights of radiological staff, patients and the public, as well as the equipment, place and protection meeting relevant standards, they can be exempted from licensing procedures for radiological diagnosis and treatment technology and medical radiation protection institutions. After the epidemic, relevant procedures must be completed according to stipulation.
As for the occupational exposure monitoring of medical personnel, individual monitoring of occupational external exposure should be strengthened following the requirements of Specifications for individual monitoring of occupational external exposure (GBZ128-2019) (12). Pay attention to the cleaning and disinfection of the dosimeters during the wearing, recycling, and monitoring. At the same time, in terms of infection monitoring, according to Technical specifications for SARS-CoV-2 detection Part 9: Occupational exposure of medical personnel detection and evaluation (DB32/T 3762.9-2020) (13), medical personnel should be regularly sampled with hand surfaces, exposed skin on the face, nasal mucosa, nasal swabs, and throat swabs, and laboratory nucleic acid testing on them should be performed. Risk assessment and tracing of positive results must be carried out. For those with positive results of hands or exposed skin, isolate medical observations should be taken and the air and surface of the workplace should be disinfected. Ask patients to take personal protection and remind doctors to do well in hand hygiene and exposed skin protection and disinfection. For those with positive results of nasal mucosa, isolate medical observations should be taken, strengthen the ventilation and disinfection of air in the hospital, remind doctors to check whether the protective equipment meets the requirements, check whether the airtightness of the medical protective mask is good or whether it is worn correctly. For those with positive results of nasal swabs or throat swabs, isolate medical observations should be taken, the symptoms of the person concerned would be closely observed, and close contacts must be found for medical isolation. Strengthening infection control management for medical personnel.
As for monitoring of workplace, according to Requirements for radiological protection in medical X-ray diagnosis (GBZ130-2013), Specification for testing of quality control in X-ray computed tomography (WS519-2019) (14) and Specification for testing of quality control in medical digital radiography (DR) systems (WS521-2017) (15), radiological protection monitoring of various types of diagnostic sites, CT and DR should be carried out. In terms of infection control, following the requirements of Technical specifications for SARS-CoV-2 detection Part 7: Air sample detection and evaluation (DB32/T 3762.7-2020) (16) and Technical specifications for SARS-CoV-2 detection Part 8: Contamination of surfaces detection and evaluation (DB32/T 3762.8-2020) (17), the air samples, the surfaces of high-frequency contact objects in the radiology work place (such as door handles, work surfaces, etc.), the surfaces easily contaminated in the toilet and the surfaces of sanitary tools should be sampled and laboratory nucleic acid testing and evaluation should be carried out.
Discussion
X-ray imaging is an important method for the diagnosis of the novel coronavirus pneumonia in the current epidemic transmission. Base on Guidelines for the prevention and control of novel coronavirus pneumonia infections in medical institutions (version 1) of National Health Commission, Jiangsu CDC refined the prevention and control measures for X-ray imaging diagnosis of the novel coronavirus pneumonia in consideration of the X-ray imaging diagnostic process. It is active and effective in cutting off the transmission route, preventing cross infection and virus spread. X-ray imaging diagnosis staff of the novel coronavirus pneumonia who exposed to SARS-CoV-2 virus should have high occupational sensitivity and strengthen self-protection measures, master prevention and control knowledge and skills, follow infection control requirements, strictly enforce hand hygiene regulations and use of personal protective equipment. The prevention and control measures can be adopted not only in this epidemic prevention and control, but also in other similar situations in the future, which has practical significance.
Diagnosis and treatment of novel coronavirus pneumonia (version 1 to 6) use imaging as one of the conditions for the diagnosis of the novel coronavirus pneumonia, the sixth edition adds the clause that “Pulmonary imaging shows significant progression of lesions over 50% within 24–48 hours” in the diagnosis of severe coronavirus pneumonia. There is no doubt that X-ray imaging plays an irreplaceable role in the diagnosis and treatment of the novel coronavirus pneumonia which gives it the legitimacy of radiation practice. However, enough attention should be paid to the control of occupational exposure and medical exposure. In practical work, the dose caused by a CT scan is dozens of times more than that by a DR radiograph, so the choice of CT scan and DR radiography should also be considered. If DR imaging can achieve the purpose of diagnosis and classification, CT scan will not be used. If a CT scan is necessary, the scan parameters should also be optimized to minimize the number of CT scans. According to Radiological protection standards for the examinee in medical X-ray diagnosis (GB16348-2010) (18), during the radiological diagnosis process, the protection of the examinee, especially the optimization of radiation protection of children, women of child-bearing age, and other special groups should be carried out. Attention should be paid to the use of protective equipment to shield the non-exposed areas of the examinee to prevent the non-inspected parts from being exposed to useful radiation.
Acknowledgments
Funding: The work was supported by Scientific Research Fund of Jiangsu Commission of Health (S2017002).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe.2020.03.05). BZ serves as an Editor-in-Chief of Journal of Public Health and Emergency. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Xinhuanet. Novel coronavirus pneumonia named as "COVID-19" by WHO. Available online: http://www.xinhuanet.com/world/2020-02/12/c_1125561389.htm, 2020.
- National Health Commission. Prevention and Control Program of novel coronavirus pneumonia (version 4). Available online: http://www.nhc.gov.cn/jkj/s3577/202002/573340613ab243b3a7f61df260551dd4/files/c791e5a7ea5149f680fdcb34dac0f54e.pdf, 2020
- National Health Commission. Diagnosis and treatment of novel coronavirus pneumonia (trial version 5). Available online: http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2/files/b218cfeb1bc54639af227f922bf6b817.pdf, 2020.
- National Health Commission. Guidelines for the prevention and control of novel coronavirus pneumonia infections in medical institutions. (version 1). Available online: http://www.nhc.gov.cn/xcs/zhengcwj/202001/b91fdab7c304431eb082d67847d27e14.shtml, 2020.
- Jiangsu Commission of Health. Guidelines for the prevention and control of infection in X-ray imaging diagnosis of novel coronavirus pneumonia infections in medical institutions in Jiangsu Province (trial version). Available online: http://www.jscdc.cn/zxzx/jkzt1/tfyjzt/xxgzbd/jsgf/202002/P020200213403993716867.pdf, 2020.
- Ng M, Lee E, Yang J, et al. Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. Radiology: Cardiothoracic imaging 2020. Available online: https://doi.org/
10.1148/ryct.2020200034 - Chung M, Adam B, Mei X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology: Cardiothoracic imaging 2020. Available online: https://doi.org/
10.1148/radiol.2020200230 - Sun QF. Salute to the radiation workers with duty to defend our land against the outbreak of novel coronavirus pneumonia. China J Radiol Med Prot 2020;40:81.
- General Administration of Quality Supervision, Inspection and Quarantine of the People's Republic of China. GB18871-2002 Basic standards for protection against ionizing radiation and for the safety of radiation sources Beijing: Standards Press of China, 2003.
- Health and Family Planning Commission of the People's Republic of China. GBZ 130-2013 Requirements for radiological protection in medical X-ray diagnosis. Beijing: Standards Press of China, 2013.
- Ministry of Health of the People's Republic of China. WS/T 367-2012 Regulation of disinfection technique in healthcare settings. Beijing: Standards Press of China, 2012.
- National Health Commission of the People's Republic of China. GBZ128-2019 Specifications for individual monitoring of occupational external exposure. Beijing: Standards Press of China, 2019.
- Jiangsu market supervision and Administration Bureau. DB32/T 3762.9-2020 Technical specifications for SARS-CoV-2 detection Part 9: Occupational exposure of medical personnel detection and evaluation. Nanjing: Jiangsu Provincial Health Standardization Technical Committee, 2020.
- Health and Family Planning Commission of the People's Republic of China. WS519-2019 Specification for testing of quality control in X-ray computed tomography. Beijing: Standards Press of China, 2019.
- Health and Family Planning Commission of the People's Republic of China. WS521-2017 Specification for testing of quality control in medical digital radiography (DR) systems. Beijing: Standards Press of China, 2017.
- Jiangsu market supervision and Administration Bureau. DB32/T 3762.7-2020 Technical specifications for SARS-CoV-2 detection Part 7: Air sample detection and evaluation. Nanjing: Jiangsu Provincial Health Standardization Technical Committee, 2020.
- Jiangsu market supervision and Administration Bureau. DB32/T 3762.8-2020 Technical specifications for SARS-CoV-2 detection Part 8: Contaminatin of surfaces detection and evaluation. Nanjing: Jiangsu Provincial Health Standardization Technical Committee, 2020.
- Ministry of Health of the People's Republic of China. GB 16348-2010 Radiological protection standards for the examinee in medical X-ray diagnosis. Beijing: Standards Press of China, 2010.
Cite this article as: Shi X, Ma J, Wang J, Yu N, Zhu B. Requirements for health prevention and control for COVID-19 during radiological diagnosis in Jiangsu Province. J Public Health Emerg 2020;4:11.