
The role of diaspora and non-governmental organization in helping Sudanese children with congenital heart diseases: 6 years’ paediatric cardiac surgery camps experience
Introduction
Congenital heart diseases (CHD) is one of the top eight diseases that lead to the death of children in Sudan as identified by the Ministry of Health in Khartoum state (1). Worldwide the incidence of CHD is about 8 in every 1,000 live born babies. Significant geographical differences were found, for instance, in Asia, the prevalence is 9.3 per 1,000, Europe 8.2 per 1,000 and North America 6.9 per 1,000 live births (2). In Sudan, some article reported that the prevalence of CHD is 0.2% (2 per 1,000 live births) in pediatric age group and about 1.5% of all deliveries diagnosed as cardiomyopathy (3). Although the prevalence is higher than the worldwide prevalence of CHD, the resources to diagnose and manage this group of ill children is so much lacking behind. There are three cardiac medical centers in Sudan. Two located in Khartoum state and the third is in Wad Madani 180 Kilometers south of Khartoum (4-8). Most of the trained physicians and surgeons are specialized for adults’ cardiac diseases. The known waiting number of children to get the proper cardiac surgery or catheter intervention is more than 1,500 children. The most challenging factors in performing cardiac operation in developing countries like Sudan are the unavailability of the well-trained medical staff and the limited necessary technical resources. This likely because the priority in the health authority strategic plans is to treat endemic disease (5-8).
Currently, there is only one well-trained pediatric cardiac surgeon in Sudan, not more than four well-trained pediatric cardiac interventionists; no well-trained graduated respiratory therapist and no well-trained specialized pediatric ICU (PICU) nurses. In addition, the PICUs are considered to be low set up regarding equipment and advanced monitoring system. Other important factors that contribute to mortality and morbidity of children with CHD are comorbidities like severe malnutrition, recurrent protozoal infections, illiteracy and low socioeconomic status. The cultural and religious background of the family has an indispensable impact in the decision of seeking a cure for their CHD children (e.g., some of them believe that such malformations created by Allah (God) should be accepted as it is).
Unfortunately, due to late diagnosis and lack of facilities, late presentation of children is always associated with complications like Eisenmenger’s syndrome or severe pulmonary hypertension that is beyond the capacities of Sudan cardiac centers to provide them the required intervention. About 10% of Down’s syndrome children with CHD having Eisenmenger’s syndrome at the time of presentation (4). The reported mortality following cardiac surgery for CHD children is 8.3% in Sudan cardiac center. Two third of the surgical intervention performed by the local medical staff and one third by visiting team over 1 year (5-8).
Methods
This initiative of helping Sudanese children with CHD was started in 2011 by some Sudanese doctors based in Doha, Qatar. This initiative was in response to the request made by the senior pediatric cardiologist in Ahmed Qasim cardiac center in Khartoum, calling for urgent help for sixty waiting children with CHD required immediate cardiac intervention. As a Sudanese pediatric intensivist and pediatric cardiologist in diaspora at Hamad Medical Corporation in Doha, Qatar we decided to move for help on a charity basis, our aim was to treat children with CHD by cardiac surgery or/and cardiac catheter interventions, to share our experience and transfer our knowledge to the local medical staff in Sudan. Also, to provide teaching and hand on training for the Sudanese medical and paramedics in the field of managing CHD children at all stages preoperative, intraoperative and postoperative. Stablishing steering committee by the diaspora physicians in Doha targeting to achieve these aims to improve the health system in Sudan and adequately reducing the mortality and morbidity of one the top eight killing diseases in children (Figure 1).
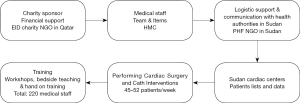
Coordination and partnership are bringing Patient Helping Fund (PHF) the most significant medical charity in Sudan, Eid Althani charity association in Qatar with the collaboration of the Federal Ministry of Health (FMH) in Sudan, Ministry of Health in Khartoum and Gazira states, we established the program of providing suitable care for in need children.
We studied the epidemiological, clinical, echocardiographic and surgical data from camps mission’s summary, from the local physician’s referrals and documents. The 30 days’ post-operative outcomes within the available PICUs resources and capabilities were assessed.
Results
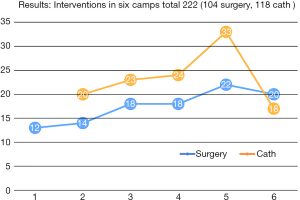
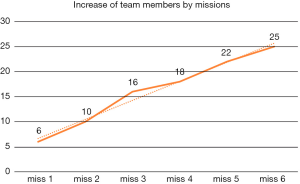
A total of 104 out of the 222 complex defects were considered for surgery, 118 underwent cardiac catheter interventions (Figure 2). With increased number of medical team, more interventions performed mission after mission (Figure 3). The 30-days post-operative mortality was 14/222 (6.3%). The most important post-surgical complications were postpericardiotomy syndrome, bleeding, and sepsis. Malnutrition poor socioeconomic status is significant factors negatively impact the outcomes (Figure 2). All surviving patients (n=208) remain in good clinical condition, and most are asymptomatic without any medications.
Discussion
Organizing cardiac camps by diaspora physicians can do a lot in form of transfer of knowledge and skills across disciplines, build upon the local capacity. It provides relevant and life-changing interventions, and immediate changes leading to sustainable longer-term developments (9). It raises up the awareness of the health authorities about the importance of dealing with CHD children by adjusting the local facilities with the help of expertise that can be recruited through a partnership between diaspora, domestic and international non-governmental organizations (NGOs). This may in part suggest at least one benefit gained from the emigration of doctors from sub-Saharan Africa (10). Although the 104 CHD children who underwent cardiac surgeries during a total of 36 working days over the six cardiac missions still the mortality rate (6.3%) is less than the reported mortality rate from Sudan cardiac centers (8.3%) (5-8). The most challenging factors in performing cardiac surgery in developing countries are the unavailability of the well-trained medical staff, limited necessary technical resources, and the absence of some rescue therapeutic measures namely inhaled nitric oxide and milrinone. The comorbidities of the endemic health problems like severe malnutrition, failure to thrive, severe nutritional anemia and chronic protozoal infections have a major adverse effect on the outcome following cardiac surgery (6,7). The cultural believes and religious background cannot be ignored. The level of training and experience of the medical team is an essential factor to get the best outcomes in low set PICU. So, build up the medical team quantity and quality wise mission after mission (from 7 members in the first mission to 22 in the Six One). Sharing and transfer knowledge and experience with the local medical staff through companied teaching rounds workshops and other educational activities during camps improved the patients’ outcomes. Some of the literature from Sudan reported that the prevalence of CHD in children is about 0.2% (2 per 1,000 live births) (3), which is low compared with the worldwide prevalence. This is most likely due to under-reporting of other cases that lived in areas where it is difficult to access any pediatric cardiac service.
Conclusions
The partnership between diaspora physicians in one hand and local and international NGOs proved to raise the awareness of the high health authorities in Sudan to adjust their local facilities with some modifications to reduce the mortality of children with underline CHD. Our experience through the six camps showed that the outcomes dramatically improved with the increase in the number of the expert medical team. More training and exposure of the local staff have a positive impact in treating children with CHD through diagnostic and therapeutic interventions. Training and education of Sudanese medical staff during the charity cardiac missions and continuity of that by different workshops and courses is one of the fundamental requirements to help CHD pediatric population in Sudan.
Acknowledgments
We would like to take this opportunity to acknowledge the support of Patient Helping Fund (PHF), Khartoum, Sudan; Eid Althani Charity Association, Qatar; The Federal Ministry of Health (FMH) in Sudan and Ministry of health in Khartoum and Gezira states. We are also very grateful to Prof. Mohamed ElSanousi Mohamed ElSanousi Vice Chancellor of University of Gezira for his unlimited support for this project and during the time of writing this manuscript.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mohamed H. Ahmed, Heitham Awadalla and Ahmed O. Almobarak) for the series “The Role of Sudanese Diaspora and NGO in Health System in Sudan” published in Journal of Public Health and Emergency. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe.2018.09.01). The series “The Role of Sudanese Diaspora and NGO in Health System in Sudan” was commissioned by the editorial office without any funding or sponsorship. MHA serves as an unpaid editorial board member of Journal of Public Health and Emergency from Aug 2017 to Jul 2019 and served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). An ethical clearance of the research was obtained from the Ethical Committee of the Faculty of Medicine, University of Gezira, Wad Medani (IRB number: 00003818), Sudan and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hayder A. Children malnutrition diseases in Sudan. Sudanel. Available online: www.sudaress.com/sudanline/34233
- van der Linde D, Konings EE, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 2011;58:2241-7. [Crossref] [PubMed]
- Suliman A. The state of heart disease in Sudan. Cardiovasc J Afr 2011;22:191-6. [Crossref] [PubMed]
- Ali SK. Cardiac abnormalities of Sudanese patients with Down's syndrome and their short-term outcome. Cardiovasc J Afr 2009;20:112-5. [PubMed]
- Tanner K, Sabrine N, Wren C. Cardiovascular malformations among preterm infants. Pediatrics 2005;116:e833-8. [Crossref] [PubMed]
- Kheir SM, Ali SK. The control of rheumatic fever and rheumatic heart disease: a call to raise the awareness. Sudan J Paediatr 2014;14:21-4. [PubMed]
- Ali SK. Rebuilding the rheumatic heart disease program in Sudan. Glob Heart 2013;8:285-6. [Crossref] [PubMed]
- Ali S, Awadallah H, Al Hamim A, et al. Handheld echocardiography for screening and control of rheumatic heart disease study in Gezira state, Sudan: a double approach model. Cardiovasc Diagn Ther 2018;8:500-7. [Crossref] [PubMed]
- Abdalla FM, Omar MA, Badr EE. Contribution of Sudanese medical diaspora to the healthcare delivery system in Sudan: exploring options and barriers. Hum Resour Health 2016;14:28. [Crossref] [PubMed]
- Mills EJ, Kanters S, Hagopian A, et al. The financial cost of doctors emigrating from sub-Saharan Africa: human capital analysis. BMJ 2011;343:d7031. [Crossref] [PubMed]
Cite this article as: Algibali OY, Juma BE, Algibaly RO, Ahmed MH. The role of diaspora and non-governmental organization in helping Sudanese children with congenital heart diseases: 6 years’ paediatric cardiac surgery camps experience. J Public Health Emerg 2018;2:26.


